Abstract
Purpose
Despite the increasing use of telemanipulators in colorectal surgery, an additional benefit in terms of improved perioperative results is not proven. The aim of the study was to compare clinical, oncological, and functional results of Da Vinci (Xi)–assisted versus conventional laparoscopic (low) anterior resection for rectal cancer.
Methods
Monocenter, prospective, controlled cohort study with a 12-month follow-up of bladder and sexual function using the validated questionnaires International Prostate Symptom Score, International Index of Erectile Function, and Female Sexual Function Index.
Results
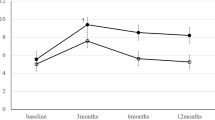
Fifty-one patients were included (18, Da Vinci (Xi) assisted; 33, conventional laparoscopy). Conversion to an open approach was more common in the Da Vinci cohort (p = 0.012). In addition, surgery and resumption of a normal diet took longer in the robotic group (p = 0.005; p = 0.042). Surgical morbidity and oncological quality did not differ. There was no difference in most functional domains, except for worsened ability to orgasm (p = 0.047) and sexual satisfaction (p = 0.034) in women after conventional laparoscopy. Moreover, we found a higher rate of improved bladder function in the conventional laparoscopy group (p = 0.023) and less painful sexual intercourse among women in the robot-assisted group (p = 0.049).
Conclusion
In contrast to the ROLARR trial, a higher conversion rate was found in the robotic cohort, which may in part be explained by a learning curve effect. Nevertheless, the Da Vinci–assisted approach showed favorable results regarding sexual function.
Similar content being viewed by others
References
Green BL, Marshall HC, Collinson F, Quirke P, Guillou P, Jayne DG, Brown JM (2013) Long-term follow-up of the Medical Research Council CLASICC trial of conventional versus laparoscopically assisted resection in colorectal cancer. Br J Surg 100(1):75–82. https://doi.org/10.1002/bjs.8945
Bonjer HJ, Deijen CL, Haglind E, Group CIS (2015) A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med 373(2):194. https://doi.org/10.1056/NEJMc1505367
Prete FP, Pezzolla A, Prete F, Testini M, Marzaioli R, Patriti A, Jimenez-Rodriguez RM, Gurrado A, Strippoli GFM (2018) Robotic versus laparoscopic minimally invasive surgery for rectal cancer: a systematic review and meta-analysis of randomized controlled trials. Ann Surg 267(6):1034–1046. https://doi.org/10.1097/SLA.0000000000002523
Barry MJ, Fowler FJ Jr, O’Leary MP, Bruskewitz RC, Holtgrewe HL, Mebust WK, Cockett AT (1992) The American Urological Association symptom index for benign prostatic hyperplasia. The Measurement Committee of the American Urological Association. J Urol 148(5):1549–1557 discussion 1564
Rosen RC, Riley A, Wagner G, Osterloh IH, Kirkpatrick J, Mishra A (1997) The international index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology 49(6):822–830
Rosen R, Brown C, Heiman J, Leiblum S, Meston C, Shabsigh R, Ferguson D, D’Agostino R Jr (2000) The Female Sexual Function Index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther 26(2):191–208. https://doi.org/10.1080/009262300278597
Thirlaway K, Fallowfield L, Cuzick J (1996) The Sexual Activity Questionnaire: a measure of women’s sexual functioning. Qual Life Res 5(1):81–90
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Jayne D, Pigazzi A, Marshall H, Croft J, Corrigan N, Copeland J, Quirke P, West N, Rautio T, Thomassen N, Tilney H, Gudgeon M, Bianchi PP, Edlin R, Hulme C, Brown J (2017) Effect of robotic-assisted vs conventional laparoscopic surgery on risk of conversion to open laparotomy among patients undergoing resection for rectal cancer: the ROLARR randomized clinical trial. JAMA 318(16):1569–1580. https://doi.org/10.1001/jama.2017.7219
Kim MJ, Park SC, Park JW, Chang HJ, Kim DY, Nam BH, Sohn DK, Oh JH (2018) Robot-assisted versus laparoscopic surgery for rectal cancer: a phase II open label prospective randomized controlled trial. Ann Surg 267(2):243–251. https://doi.org/10.1097/SLA.0000000000002321
Hardt J, Pilz L, Magdeburg J, Kienle P, Post S, Magdeburg R (2017) Preoperative hypoalbuminemia is an independent risk factor for increased high-grade morbidity after elective rectal cancer resection. Int J Color Dis 32(10):1439–1446. https://doi.org/10.1007/s00384-017-2884-7
Jimenez-Rodriguez RM, Rubio-Dorado-Manzanares M, Diaz-Pavon JM, Reyes-Diaz ML, Vazquez-Monchul JM, Garcia-Cabrera AM, Padillo J, De la Portilla F (2016) Learning curve in robotic rectal cancer surgery: current state of affairs. Int J Color Dis 31(12):1807–1815. https://doi.org/10.1007/s00384-016-2660-0
Odermatt M, Ahmed J, Panteleimonitis S, Khan J, Parvaiz A (2017) Prior experience in laparoscopic rectal surgery can minimise the learning curve for robotic rectal resections: a cumulative sum analysis. Surg Endosc 31(10):4067–4076. https://doi.org/10.1007/s00464-017-5453-9
Kim JY, Kim NK, Lee KY, Hur H, Min BS, Kim JH (2012) A comparative study of voiding and sexual function after total mesorectal excision with autonomic nerve preservation for rectal cancer: laparoscopic versus robotic surgery. Ann Surg Oncol 19(8):2485–2493. https://doi.org/10.1245/s10434-012-2262-1
D’Annibale A, Pernazza G, Monsellato I, Pende V, Lucandri G, Mazzocchi P, Alfano G (2013) Total mesorectal excision: a comparison of oncological and functional outcomes between robotic and laparoscopic surgery for rectal cancer. Surg Endosc 27(6):1887–1895. https://doi.org/10.1007/s00464-012-2731-4
Morelli L, Ceccarelli C, Di Franco G, Guadagni S, Palmeri M, Caprili G, D’Isidoro C, Marciano E, Pollina L, Campani D, Massimetti G, Di Candio G, Mosca F (2016) Sexual and urinary functions after robot-assisted versus pure laparoscopic total mesorectal excision for rectal cancer. Int J Color Dis 31(4):913–915. https://doi.org/10.1007/s00384-015-2301-z
Panteleimonitis S, Ahmed J, Ramachandra M, Farooq M, Harper M, Parvaiz A (2017) Urogenital function in robotic vs laparoscopic rectal cancer surgery: a comparative study. Int J Color Dis 32(2):241–248. https://doi.org/10.1007/s00384-016-2682-7
Authorship and contributions
J. Hardt, C. Galata, G. Vassilev, P. Kienle, C. Reißfelder: conceived of the study
J. Hardt, F. Haas, S. Büttner: acquired and analyzed the data
All authors interpreted the data, revised the article for important intellectual content, and gave final approval of the version to be published.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The trial received institutional ethical approval by the ethics committee of the Medical Faculty Mannheim, Heidelberg University, Mannheim, Germany (2015-636 N-MA). The study was performed according to the Declaration of Helsinki. All participants provided written informed consent.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Galata, C., Vassilev, G., Haas, F. et al. Clinical, oncological, and functional outcomes of Da Vinci (Xi)–assisted versus conventional laparoscopic resection for rectal cancer: a prospective, controlled cohort study of 51 consecutive cases. Int J Colorectal Dis 34, 1907–1914 (2019). https://doi.org/10.1007/s00384-019-03397-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-019-03397-w