Abstract
Purpose
Surgical site infections (SSIs) have become a leading cause of preventable morbidity and mortality in surgery. The aim was to evaluate the efficacy of a dual-ring wound protector to prevent the SSIs in Crohn’s disease (CD) after bowel resection.
Methods
This retrospective observational study included all CD patients undergoing bowel resection at the Inflammatory Bowel Disease Center between January 2015 and June 2018 at Sir Run Run Shaw Hospital. Risk factors of SSIs were evaluated by assessing preoperative clinical characteristics and perioperative treatments in univariate and multivariate analyses. Outcomes for CD patients with and without the wound protector were compared.
Results
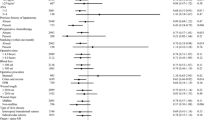
Three hundred forty-four CD patients were enrolled in this study, 121 (35.2%) patients had postoperative complications, of whom, 72 (20.9%) patients developed SSIs (12.8% patients with incisional SSI and 8.1% patients with organ/space SSI). There was a significant reduction in the incidence of incisional SSI in the wound protector group (8.1% vs 16.8%, p < 0.05). No significant differences were identified in organ/space SSI between groups with and without wound protector (6.3% vs 9.8%, p = 0.232). Incisional SSI correlated with preoperative albumin, C-reactive protein, white blood cell, age (≤ 16), penetrating disease behavior, surgical history, open surgery, stoma creation, estimated blood loss, infliximab, and wound protector (p < 0.05). Multivariate analysis identified the wound protector to be one of independent factors for preventing incisional SSIs (OR 0.357, 95% CI 0.161–0.793, p < 0.05).
Conclusion
Among the CD patients with bowel resection, the use of a dual-ring wound protector during surgery significantly reduced the risk of incisional SSI.

Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the first author or corresponding author on reasonable request.
References
Torres J, Mehandru S, Colombel JF, Peyrin-Biroulet L (2017) Crohn's disease. Lancet 389(10080):1741–1755. https://doi.org/10.1016/S0140-6736(16)31711-1
Liu W, Zhou W, Xiang J, Cao Q, Zhu J, Qi W, Chen P, Xie Q (2018) Lemann index at diagnosis predicts the risk of early surgery in Crohn’s disease. Dis Colon Rectum 61(2):207–213. https://doi.org/10.1097/DCR.0000000000000930
Regueiro M, Schraut W, Baidoo L, Kip KE, Sepulveda AR, Pesci M, Harrison J, Plevy SE (2009) Infliximab prevents Crohn’s disease recurrence after ileal resection. Gastroenterology 136(2):441–450 e441; quiz 716. https://doi.org/10.1053/j.gastro.2008.10.051
Shen B (2017) IBD: step-up vs top-down therapy for Crohn’s disease: medicine vs surgery. Nat Rev Gastroenterol Hepatol 14(12):693–695. https://doi.org/10.1038/nrgastro.2017.139
Ponsioen CY, de Groof EJ, Eshuis EJ, Gardenbroek TJ, Bossuyt PMM, Hart A, Warusavitarne J, Buskens CJ, van Bodegraven AA, Brink MA, ECJ C, van Wagensveld BA, MCM R, Crolla R, Noomen CG, Houdijk APJ, Mallant RC, Boom M, Marsman WA, Stockmann HB, Mol B, de Groof AJ, Stokkers PC, D’Haens GRR, Bemelman WA, group LCs (2017) Laparoscopic ileocaecal resection versus infliximab for terminal ileitis in Crohn’s disease: a randomised controlled, open-label, multicentre trial. Lancet Gastroenterol Hepatol 2(11):785–792. https://doi.org/10.1016/S2468-1253(17)30248-0
Fumery M, Seksik P, Auzolle C, Munoz-Bongrand N, Gornet JM, Boschetti G, Cotte E, Buisson A, Dubois A, Pariente B, Zerbib P, Chafai N, Stefanescu C, Panis Y, Marteau P, Pautrat K, Sabbagh C, Filippi J, Chevrier M, Houze P, Jouven X, Treton X, Allez M, investigators Rsg (2017) Postoperative complications after ileocecal resection in Crohn’s disease: a prospective study from the REMIND group. Am J Gastroenterol 112(2):337–345. https://doi.org/10.1038/ajg.2016.541
Zuo L, Li Y, Wang H, Zhu W, Zhang W, Gong J, Li N, Li J (2015) A practical predictive index for intra-abdominal septic complications after primary anastomosis for Crohn’s disease: change in C-reactive protein level before surgery. Dis Colon Rectum 58(8):775–781. https://doi.org/10.1097/DCR.0000000000000414
Uchino M, Ikeuchi H, Tsuchida T, Nakajima K, Tomita N, Takesue Y (2009) Surgical site infection following surgery for inflammatory bowel disease in patients with clean-contaminated wounds. World J Surg 33(5):1042–1048. https://doi.org/10.1007/s00268-009-9934-4
Bhakta A, Tafen M, Glotzer O, Ata A, Chismark AD, Valerian BT, Stain SC, Lee EC (2016) Increased incidence of surgical site infection in IBD patients. Dis Colon Rectum 59(4):316–322. https://doi.org/10.1097/DCR.0000000000000550
Weiss CA 3rd, Statz CL, Dahms RA, Remucal MJ, Dunn DL, Beilman GJ (1999) Six years of surgical wound infection surveillance at a tertiary care center: review of the microbiologic and epidemiological aspects of 20,007 wounds. Arch Surg 134(10):1041–1048
Bressan AK, Aubin JM, Martel G, Dixon E, Bathe OF, Sutherland FR, Balaa F, Mimeault R, Edwards JP, Grondin SC, Isherwood S, Lillemoe KD, Saeed S, Ball CG (2018) Efficacy of a dual-ring wound protector for prevention of surgical site infections after pancreaticoduodenectomy in patients with intrabiliary stents: a randomized clinical trial. Ann Surg 268(1):35–40. https://doi.org/10.1097/SLA.0000000000002614
Pinkney TD, Calvert M, Bartlett DC, Gheorghe A, Redman V, Dowswell G, Hawkins W, Mak T, Youssef H, Richardson C, Hornby S, Magill L, Haslop R, Wilson S, Morton D, West Midlands Research C, Investigators RT (2013) Impact of wound edge protection devices on surgical site infection after laparotomy: multicentre randomised controlled trial (ROSSINI trial). Bmj 347:f4305. https://doi.org/10.1136/bmj.f4305
Reid K, Pockney P, Draganic B, Smith SR (2010) Barrier wound protection decreases surgical site infection in open elective colorectal surgery: a randomized clinical trial. Dis Colon Rectum 53(10):1374–1380. https://doi.org/10.1007/DCR.0b013e3181ed3f7e
Gheorghe A, Calvert M, Pinkney TD, Fletcher BR, Bartlett DC, Hawkins WJ, Mak T, Youssef H, Wilson S, West Midlands Research C, Group RTM (2012) Systematic review of the clinical effectiveness of wound-edge protection devices in reducing surgical site infection in patients undergoing open abdominal surgery. Ann Surg 255(6):1017–1029. https://doi.org/10.1097/SLA.0b013e31823e7411
Luo Y, Qiu YE, Mu YF, Qin SL, Qi Y, Zhong M, Yu MH, Ma LY (2017) Plastic wound protectors decreased surgical site infections following laparoscopic-assisted colectomy for colorectal cancer: a retrospective cohort study. Medicine 96(37):e7752. https://doi.org/10.1097/MD.0000000000007752
Allegranzi B, Bischoff P, de Jonge S, Kubilay NZ, Zayed B, Gomes SM, Abbas M, Atema JJ, Gans S, van Rijen M, Boermeester MA, Egger M, Kluytmans J, Pittet D, Solomkin JS, Group WHOGD (2016) New WHO recommendations on preoperative measures for surgical site infection prevention: an evidence-based global perspective. Lancet Infect Dis 16(12):e276–e287. https://doi.org/10.1016/S1473-3099(16)30398-X
Hedrick TL, Harrigan AM, Sawyer RG, Turrentine FE, Stukenborg GJ, Umapathi BA, Friel CM (2015) Defining surgical site infection in colorectal surgery: an objective analysis using serial photographic documentation. Dis Colon Rectum 58(11):1070–1077. https://doi.org/10.1097/DCR.0000000000000466
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Ge X, Dai X, Ding C, Tian H, Yang J, Gong J, Zhu W, Li N, Li J (2017) Early postoperative decrease of serum albumin predicts surgical outcome in patients undergoing colorectal resection. Dis Colon Rectum 60(3):326–334. https://doi.org/10.1097/DCR.0000000000000750
Satsangi J, Silverberg MS, Vermeire S, Colombel JF (2006) The Montreal classification of inflammatory bowel disease: controversies, consensus, and implications. Gut 55(6):749–753. https://doi.org/10.1136/gut.2005.082909
Maeda K, Nagahara H, Shibutani M, Otani H, Sakurai K, Toyokawa T, Tanaka H, Kubo N, Muguruma K, Kamata N, Yamagami H, Hirakawa K (2015) A preoperative low nutritional prognostic index correlates with the incidence of incisional surgical site infections after bowel resection in patients with Crohn’s disease. Surg Today 45(11):1366–1372. https://doi.org/10.1007/s00595-014-1044-8
Krizek TJ, Robson MC (1975) Evolution of quantitative bacteriology in wound management. Am J Surg 130(5):579–584
Mohan HM, Mcdermott S, Fenelon L, Fearon NM, O’Connell PR, Oon SF, Burke J, Keane E, Shields C, Winter DC, Members of the University College Dublin Wound Retractor Study G (2012) Plastic wound retractors as bacteriological barriers in gastrointestinal surgery: a prospective multi-institutional trial. J Hosp Infect 81(2):109–113. https://doi.org/10.1016/j.jhin.2012.03.005
Horiuchi T, Tanishima H, Tamagawa K, Sakaguchi S, Shono Y, Tsubakihara H, Tabuse K, Kinoshita Y (2010) A wound protector shields incision sites from bacterial invasion. Surg Infect 11(6):501–503. https://doi.org/10.1089/sur.2009.072
Gabrielsen J, Petrick A, Ibele A, Wood GC, Benotti P (2014) A novel technique for wound protector deployment and efficient specimen extraction following laparoscopic sleeve gastrectomy. J Gastrointest Surg 18(9):1678–1682. https://doi.org/10.1007/s11605-014-2512-6
Uchino M, Ikeuchi H, Bando T, Chohno T, Sasaki H, Horio Y, Nakajima K, Takesue Y (2017) Efficacy of preoperative oral antibiotic prophylaxis for the prevention of surgical site infections in patients with Crohn disease: a randomized controlled trial. Ann Surg 269:420–426. https://doi.org/10.1097/SLA.0000000000002567
Uchino M, Ikeuchi H, Matsuoka H, Bando T, Ichiki K, Nakajima K, Tomita N, Takesue Y (2013) Risk factors for surgical site infection and association with infliximab administration during surgery for Crohn’s disease. Dis Colon Rectum 56(10):1156–1165. https://doi.org/10.1097/DCR.0b013e31829f682c
Lightner AL, Mathis KL, Tse CS, Pemberton JH, Shen B, Kochlar G, Singh A, Dulai PS, Eisenstein S, Sandborn WJ, Parry L, Stringfield S, Hudesman D, Remzi F, Loftus EV Jr (2018) Postoperative outcomes in vedolizumab-treated patients undergoing major abdominal operations for inflammatory bowel disease: retrospective multicenter cohort study. Inflamm Bowel Dis 24(4):871–876. https://doi.org/10.1093/ibd/izx076
Brouquet A, Maggiori L, Zerbib P, Lefevre JH, Denost Q, Germain A, Cotte E, Beyer-Berjot L, Munoz-Bongrand N, Desfourneaux V, Rahili A, Duffas JP, Pautrat K, Denet C, Bridoux V, Meurette G, Faucheron JL, Loriau J, Guillon F, Vicaut E, Benoist S, Panis Y, group Gc (2018) Anti-TNF therapy is associated with an increased risk of postoperative morbidity after surgery for ileocolonic Crohn disease: results of a prospective nationwide cohort. Ann Surg 267(2):221–228. https://doi.org/10.1097/SLA.0000000000002017
Wilson MZ, Connelly TM, Hollenbeak CS, Messaris E (2014) Organ space infection following ileocolectomy for Crohn’s disease: a National Surgical Quality Improvement Project study. Am J Surg 208(5):749–755. https://doi.org/10.1016/j.amjsurg.2014.04.010
Serradori T, Germain A, Scherrer ML, Ayav C, Perez M, Romain B, Palot JP, Rohr S, Peyrin-Biroulet L, Bresler L (2013) The effect of immune therapy on surgical site infection following Crohn’s disease resection. Br J Surg 100(8):1089–1093. https://doi.org/10.1002/bjs.9152
Ikeshima R, Mizushima T, Takahashi H, Haraguchi N, Nishimura J, Hata T, Matsuda C, Ikenaga M, Nakajima K, Yamamoto H, Murata K, Doki Y, Mori M (2018) The efficacy of active drainage for preventing postoperative organ/space surgical site infections in patients with Crohn’s disease. Surg Today 48(1):25–32. https://doi.org/10.1007/s00595-017-1549-z
Patel KV, Darakhshan AA, Griffin N, Williams AB, Sanderson JD, Irving PM (2016) Patient optimization for surgery relating to Crohn’s disease. Nat Rev Gastroenterol Hepatol 13(12):707–719. https://doi.org/10.1038/nrgastro.2016.158
Levy SM, Holzmann-Pazgal G, Lally KP, Davis K, Kao LS, Tsao K (2013) Quality check of a quality measure: surgical wound classification discrepancies impact risk-stratified surgical site infection rates in pediatric appendicitis. J Am Coll Surg 217(6):969–973. https://doi.org/10.1016/j.jamcollsurg.2013.07.398
Cosnes J, Bourrier A, Nion-Larmurier I, Sokol H, Beaugerie L, Seksik P (2012) Factors affecting outcomes in Crohn’s disease over 15 years. Gut 61(8):1140–1145. https://doi.org/10.1136/gutjnl-2011-301971
Romy S, Eisenring MC, Bettschart V, Petignat C, Francioli P, Troillet N (2008) Laparoscope use and surgical site infections in digestive surgery. Ann Surg 247(4):627–632. https://doi.org/10.1097/SLA.0b013e3181638609
Drosdeck J, Harzman A, Suzo A, Arnold M, Abdel-Rasoul M, Husain S (2013) Multivariate analysis of risk factors for surgical site infection after laparoscopic colorectal surgery. Surg Endosc 27(12):4574–4580. https://doi.org/10.1007/s00464-013-3126-x
Acknowledgements
The authors gratefully acknowledge all of the investigators for their contributions to the trial, as well as Bin Chen, who provided medical writing assistance.
Funding
Supported by grants from National Natural Science Foundation of China (81800474) and Zhejiang Natural Science Foundation (LY18H030006).
Author information
Authors and Affiliations
Contributions
Xiaolong Ge and Wei Zhou contributed to the study conception and design, Xiaolong Ge, Weilin Qi, and Shasha Tang contributed to the acquisition of data, Wei Liu and Jiemin Lv contributed to the analysis and interpretation of data, Xiaolong Ge and Shasha Tang contributed to the drafting of manuscript, and Qian Cao, Xiujun Cai, and Wei Zhou contributed to the critical revision.
Corresponding author
Ethics declarations
The institutional review board of Sir Run Run Shaw Hospital approved the project.
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ge, X., Tang, S., Qi, W. et al. Prevalence and predictors of surgical site infections after bowel resection for Crohn’s disease: the role of dual-ring wound protector. Int J Colorectal Dis 34, 879–887 (2019). https://doi.org/10.1007/s00384-019-03275-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-019-03275-5