Abstract
Purpose
We report an unusual case of endometriosis of the appendix with simultaneous invasion of the sigmoid colon.
Methods
Clinical, radiological, surgical, and histological data of the patient were reviewed, as well as the current literature on gastrointestinal endometriosis.
Results
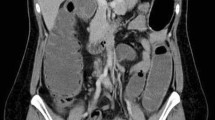
A 41-year-old woman presented to the emergency department of our hospital with acute right lower quadrant pain, pronounced tenderness elevated white blood cell count, and increased C-reactive protein. Abdominal CT scan suggested a mucocele of the appendix. The patient was first treated with antibiotics, followed by en bloc resection of the appendix and of the sigmoid colon 2 months later. Histological examination revealed an endometriotic nodule of the appendix filling the appendiceal lumen and resulting in a mucocele which invaded the sigmoid colon wall.
Conclusions
The diagnosis of gastrointestinal endometriosis can be challenging due to the variety of symptoms it can produce. Although extremely rare, a concomitant double gastrointestinal location of endometriosis may be possible and should be considered in women of reproductive age.



Similar content being viewed by others
References
Giudice LC (2010) Clinical practice. Endometriosis. N Engl J Med 362:2389–2398
Tai FW, Chang CY, Chiang JH, Lin WC, Wan L (2018) Association of pelvic inflammatory disease with risk of endometriosis: a nationwide cohort study involving 141,460 individuals. J Clin Med 7. https://doi.org/10.3390/jcm7110379
Chamie LP, Ribeiro D, Tiferes DA, Macedo Neto AC, Serafini PC (2018) Atypical sites of deeply infiltrative endometriosis: clinical characteristics and imaging findings. Radiographics 38:309–328
Charatsi D, Koukoura O, Ntavela IG, Chintziou F, Gkorila G, Tsagkoulis M, Mikos T, Pistofidis G, Hajiioannou J, Daponte A (2018) Gastrointestinal and urinary tract endometriosis: a review on the commonest locations of extrapelvic endometriosis. Adv Med 2018:3461209
Klingbeil KD, Azab B, Moller MG (2017) Low-grade appendiceal mucinous neoplasm and endometriosis of the appendix. World J Surg Oncol 15:226
Gustofson RL, Kim N, Liu S, Stratton P (2006) Endometriosis and the appendix: a case series and comprehensive review of the literature. Fertil Steril 86:298–303
Giudice LC, Kao LC (2004) Endometriosis. Lancet 364:1789–1799
Young S, Burns MK, DiFrancesco L, Nezhat A, Nezhat C (2017) Diagnostic and treatment guidelines for gastrointestinal and genitourinary endometriosis. J Turk Ger Gynecol Assoc 18:200–209
Burney RO, Giudice LC (2012) Pathogenesis and pathophysiology of endometriosis. Fertil Steril 98:511–519
Sasson IE, Taylor HS (2008) Stem cells and the pathogenesis of endometriosis. Ann N Y Acad Sci 1127:106–115
Tong YL, Chen Y, Zhu SY (2013) Ileocecal endometriosis and a diagnosis dilemma: a case report and literature review. World J Gastroenterol 19:3707–3710
Torralba-Moron A, Urbanowicz M, Ibarrola-De Andres C, Lopez-Alonso G, Colina-Ruizdelgado F, Guerra-Vales JM (2016) Acute small bowel obstruction and small bowel perforation as a clinical debut of intestinal endometriosis: a report of four cases and review of the literature. Intern Med 55:2595–2599
Vercellini P, Vigano P, Somigliana E, Fedele L (2014) Endometriosis: pathogenesis and treatment. Nat Rev Endocrinol 10:261–275
Aho AJ, Heinonen R, Lauren P (1973) Benign and malignant mucocele of the appendix. Histological types and prognosis. Acta Chir Scand 139:392–400
Rymer B, Forsythe RO, Husada G (2015) Mucocoele and mucinous tumours of the appendix: a review of the literature. Int J Surg 18:132–135
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lainas, P., Dammaro, C., Rodda, G.A. et al. Appendiceal endometriosis invading the sigmoid colon: a rare entity. Int J Colorectal Dis 34, 1147–1150 (2019). https://doi.org/10.1007/s00384-019-03242-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-019-03242-0