Abstract
Purpose
There is a significant risk of surgical resection during the lifetime of an inflammatory bowel disease (IBD) patient: laparoscopic surgery has been increasingly applied to the management of IBD with short and long-term advantages. The aim of this study is to demonstrate that laparoscopic surgery for IBD, performed by a surgical trainee under the supervision of an experienced trainer, is feasible and safe.
Methods
All surgical procedures were sub-divided in six critical steps in order to define the procedure as supervised trainee performed (STP) when the trainer was present unscrubbed in the theatre or assisting and trainer performed (TNER) when the trainer performed two or more critical steps of the procedure. Included were all patients undergoing laparoscopic resection for IBD between January 2009 and December 2013. Thirty-day mortality and morbidity were the primary outcomes. Reoperations and rehospitalizations within 30 days of discharge were recorded prospectively and were the secondary outcomes together with conversion rate and length of hospital stay.
Results
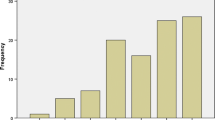
One hundred fifty-one patients were included: 77 (50.99 %) STP and 74 (49.01 %) TNER. No deaths occurred, and 30-day morbidity was 27.15 % with no differences between the groups. Operating time was longer in the STP (166.6 ± 53.31 vs 130.4 ± 49.15). Five patients (2 vs 3) required reoperation (3.31 %), while 13 patients (8.6 %) required readmission.
Conclusions
Laparoscopic surgery for IBD performed by a supervised trainee is safe compared to trainers performed procedures despite a longer operating time. Randomized clinical trials are needed to confirm these preliminary results and to investigate long-term outcomes.


Similar content being viewed by others
References
Milsom JW (2005) Laparoscopic surgery in the treatment of Crohn’s disease. Surg Clin N Am 85:25–34
Hasegawa H, Watanabe M, Nishibori H et al (2003) Laparoscopic surgery for recurrent Crohn’s disease. Br J Surg 90:970–973
Maggiori L, Khayat A, Treton X et al (2014) Laparoscopic approach for inflammatory bowel disease is a real alternative to open surgery: an experience with 574 consecutive patients. Ann Surg 260(2):305–310
Rosman AS, Melis M, Fichera A (2005) Metaanalysis of trials comparing laparoscopic and open surgery for Crohn’s disease. Surg Endosc 19:1549–1555
Tan JJ, Tjandra JJ (2006) Laparoscopic surgery for ulcerative colitis: a meta-analysis. Colorectal Dis 8:626–636
Tan JJY, Tjandra JJ (2007) Laparoscopic surgery for Crohn’s disease: a meta-analysis. Dis Colon Rectum 50:576–585
Braga M, Vignali A et al (2002) Laparoscopic versus open colorectal surgery: a randomised trial on short-term outcome. Ann Surg 236:759–766
Indar AA, Efron JE, Young-Fadok TM (2009) Laparoscopic ileal pouch-anal anastomosis reduces abdominal and pelvic adhesions. Surg Endosc 23:174–177
Taylor GW, Jayne DG, Brown SR et al (2010) Adhesions and incisional hernias following laparoscopic versus open surgery for colorectal cancer in the CLASICC trial. Br J Surg 97:70–78
Schlachta CM, Mamazza J, Seshadri PA et al (2001) Defining a learning curve for laparoscopic resections. Dis Colon Rectum 44:217–222
Lu KC, Cone MM, Diggs BS et al (2011) Laparoscopic converted to open colectomy: predictors and outcomes from the Nationwide Inpatient Sample. Am J Surg 201(5):634–639
Tekkis PP, Senagore AJ, Delaney CP et al (2005) Evaluation of the learning curve in laparoscopic colorectal surgery: comparison of right-sided and left-sided resections. Ann Surg 242:83–91
Barrie J, Jayne DG, Wright J et al (2014) Attaining surgical competency and its implications in surgical clinical trial design: a systematic review of the learning curve in laparoscopic and robot-assisted laparoscopic colorectal cancer surgery. Ann Surg Oncol 21:829–840
Miskovic D, Ni M, Wyles SM, Tekkis PP, Hanna GB (2012) Learning curve and case selection in laparoscopic colorectal surgery: systematic review and international multicenter analysis of 4852 cases. Dis Colon Rectum 55(12):1300–1310
Mackenzie H, Miskovic D, Ni M et al (2013) Clinical and educational proficiency gain of supervised laparoscopic colorectal surgical trainees. Surg Endosc 27(8):2704–2711
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Teeuwen PH, Stommel MW, Bremers et al (2009) Colectomy in patients with acute colitis: a systematic review. J Gastrointest Surg 13:678–686
Hewett PJ, Allardyce RA, Bagshaw PF et al (2008) Short-term outcomes of the Australasian randomized clinical study comparing laparoscopic and conventional open surgical treatments for colon cancer: the ALCCaS trial. Ann Surg 248:728–738
Yamamoto T, Allan RN, Keighley MR (2000) Risk factors for intra-abdominal sepsis after surgery in Crohn’s disease. Dis Colon Rectum 43:1141–1145
Marusch F, Gastinger I, Schneider C et al (2001) Importance of conversion for results obtained with laparoscopic colorectal surgery. Dis Colon Rectum 44:207–214
Conflict of interest
The authors declare no conflict of interest.
Authors’ contributions
Valerio Celentano was responsible for the conception and design of the study, analysis and interpretation of data, article drafting and review; David Finch was responsible for the acquisition of data and drafting the article; Luke Forster was responsible for the acquisition of data and drafting the article; Jonathan Robinson did the acquisition, analysis and interpretation of data and article review; and John Griffith did the conception and design of the study and article review.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Celentano, V., Finch, D., Forster, L. et al. Safety of supervised trainee-performed laparoscopic surgery for inflammatory bowel disease. Int J Colorectal Dis 30, 639–644 (2015). https://doi.org/10.1007/s00384-015-2147-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-015-2147-4