Abstract
Purpose
This study aims to determine the risk factors for lateral pelvic recurrence (LPR) in rectal cancer patients treated with neoadjuvant chemoradiotherapy (CRT) and curative surgery.
Methods
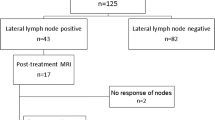
Four hundred forty-three patients treated with neoadjuvant CRT and curative surgery from October 1999 through June 2009 were analyzed. All patients underwent total mesorectal resection without lateral pelvic lymph node (LPLN) dissection. Recurrence patterns and lateral pelvic recurrence-free survival (LPFS) were evaluated relative to clinicopathologic parameters including pelvic LN status.
Results
Median follow-up was 52 months, with locoregional recurrence in 53 patients (11.9 %). Of the 53 patients, 28 (52.8 %) developed LPR, of which eight had both central and lateral PR. Multivariate analysis showed a significant relationship between LPFS and the number of lateral pelvic LN (p = 0.010) as well as the ratio of the number of positive LN/number of dissected LN (p = 0.038). The relationship between LPFS and LPLN size had a marginal trend (p = 0.085). Logistic regression analysis showed positive relationships between LPR probability and the number of LPLN (odds ratio [OR] 1.507; 95 % confidence interval [CI] 1.177–1.929; p = 0.001) as well as LPLN size (OR 1.124; CI 1.029–1.227, p = 0.009).
Conclusions
LPLN ≥ 2 and a ratio of the number of positive LN/number of dissected LN > 0.3 were prognostic of poor LPFS. The prediction curve of LPR according to the number and size of LPLN could be useful for determining the benefit of additional lateral pelvic treatment.
Access this article
We’re sorry, something doesn't seem to be working properly.
Please try refreshing the page. If that doesn't work, please contact support so we can address the problem.



Similar content being viewed by others
References
Bolognese A, Cardi M, Muttillo IA, Barbarosos A, Bocchetti T, Valabrega S (2000) Total mesorectal excision for surgical treatment of rectal cancer. J Surg Oncol 74:21–23
How P, Shihab O, Tekkis P, Brown G, Quirke P, Heald R, Moran B (2011) A systematic review of cancer related patient outcomes after anterior resection and abdominoperineal excision for rectal cancer in the total mesorectal excision era. Surg Oncol 20:e149–155
Peeters KC, Marijnen CA, Nagtegaal ID, Kranenbarg EK, Putter H, Wiggers T, Rutten H, Pahlman L, Glimelius B, Leer JW, van de Velde CJ (2007) The TME trial after a median follow-up of 6 years: increased local control but no survival benefit in irradiated patients with resectable rectal carcinoma. Ann Surg 246:693–701
Sauer R, Becker H, Hohenberger W, Rodel C, Wittekind C, Fietkau R, Martus P, Tschmelitsch J, Hager E, Hess CF, Karstens JH, Liersch T, Schmidberger H, Raab R (2004) Preoperative versus postoperative chemoradiotherapy for rectal cancer. N Engl J Med 351:1731–1740
Choi CH, Kim WD, Lee SJ, Park WY (2012) Clinical predictive factors of pathologic tumor response after preoperative chemoradiotherapy in rectal cancer. Radiat Oncol J 30:99–107
Koch M, Kienle P, Antolovic D, Buchler MW, Weitz J (2005) Is the lateral lymph node compartment relevant? Recent Results Cancer Res 165:40–45
Fujita S, Akasu T, Mizusawa J, Saito N, Kinugasa Y, Kanemitsu Y, Ohue M, Fujii S, Shiozawa M, Yamaguchi T, Moriya Y (2012) Postoperative morbidity and mortality after mesorectal excision with and without lateral lymph node dissection for clinical stage II or stage III lower rectal cancer (JCOG0212): results from a multicentre, randomised controlled, non-inferiority trial. Lancet Oncol 13:616–621
Nakamura T, Watanabe M (2013) Lateral lymph node dissection for lower rectal cancer. World J Surg 37:1808–1813
Sugihara K, Kobayashi H, Kato T, Mori T, Mochizuki H, Kameoka S, Shirouzu K, Muto T (2006) Indication and benefit of pelvic sidewall dissection for rectal cancer. Dis Colon Rectum 49:1663–1672
Kim TH, Jeong SY, Choi DH, Kim DY, Jung KH, Moon SH, Chang HJ, Lim SB, Choi HS, Park JG (2008) Lateral lymph node metastasis is a major cause of locoregional recurrence in rectal cancer treated with preoperative chemoradiotherapy and curative resection. Ann Surg Oncol 15:729–737
Yano H, Moran BJ (2008) The incidence of lateral pelvic side-wall nodal involvement in low rectal cancer may be similar in Japan and the West. Br J Surg 95:33–49
Sato H, Maeda K, Maruta M (2011) Prognostic significance of lateral lymph node dissection in node positive low rectal carcinoma. Int J Colorectal Dis 26:881–889
Ueno H, Mochizuki H, Hashiguchi Y, Hase K (2001) Prognostic determinants of patients with lateral nodal involvement by rectal cancer. Ann Surg 234:190–197
Nagawa H, Muto T, Sunouchi K, Higuchi Y, Tsurita G, Watanabe T, Sawada T (2001) Randomized, controlled trial of lateral node dissection vs. nerve-preserving resection in patients with rectal cancer after preoperative radiotherapy. Dis Colon Rectum 44:1274–1280
Georgiou P, Tan E, Gouvas N, Antoniou A, Brown G, Nicholls RJ, Tekkis P (2009) Extended lymphadenectomy versus conventional surgery for rectal cancer: a meta-analysis. Lancet Oncol 10:1053–1062
Akiyoshi T, Watanabe T, Miyata S, Kotake K, Muto T, Sugihara K (2012) Results of a Japanese nationwide multi-institutional study on lateral pelvic lymph node metastasis in low rectal cancer: is it regional or distant disease? Ann Surg 255:1129–1134
Nelson H, Petrelli N, Carlin A, Couture J, Fleshman J, Guillem J, Miedema B, Ota D, Sargent D (2001) Guidelines 2000 for colon and rectal cancer surgery. J Natl Cancer Inst 93:583–596
Moore HG, Shoup M, Riedel E, Minsky BD, Alektiar KM, Ercolani M, Paty PB, Wong WD, Guillem JG (2004) Colorectal cancer pelvic recurrences: determinants of resectability. Dis Colon Rectum 47:1599–1606
Yamada K, Ishizawa T, Niwa K, Chuman Y, Akiba S, Aikou T (2001) Patterns of pelvic invasion are prognostic in the treatment of locally recurrent rectal cancer. Br J Surg 88:988–993
Ueno M, Oya M, Azekura K, Yamaguchi T, Muto T (2005) Incidence and prognostic significance of lateral lymph node metastasis in patients with advanced low rectal cancer. Br J Surg 92:756–763
Arii K, Takifuji K, Yokoyama S, Matsuda K, Higashiguchi T, Tominaga T, Oku Y, Tani M, Yamaue H (2006) Preoperative evaluation of pelvic lateral lymph node of patients with lower rectal cancer: comparison study of MR imaging and CT in 53 patients. Langenbecks Arch Surg 391:449–454
Fujita S, Yamamoto S, Akasu T, Moriya Y (2009) Risk factors of lateral pelvic lymph node metastasis in advanced rectal cancer. Int J Colorectal Dis 24:1085–1090
Tan KY, Yamamoto S, Fujita S, Akasu T, Moriya Y (2010) Improving prediction of lateral node spread in low rectal cancers—multivariate analysis of clinicopathological factors in 1,046 cases. Langenbecks Arch Surg 395:545–549
Dharmarajan S, Shuai D, Fajardo AD, Birnbaum EH, Hunt SR, Mutch MG, Fleshman JW, Lin AY (2011) Clinically enlarged lateral pelvic lymph nodes do not influence prognosis after neoadjuvant therapy and TME in stage III rectal cancer. J Gastrointest Surg 15:1368–1374
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, T.G., Park, W., Choi, D.H. et al. Factors associated with lateral pelvic recurrence after curative resection following neoadjuvant chemoradiotherapy in rectal cancer patients. Int J Colorectal Dis 29, 193–200 (2014). https://doi.org/10.1007/s00384-013-1797-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-013-1797-3