Abstract
Purpose
The aims of the study were to describe the follow-up of colorectal cancer (CRC) patients in southern Netherlands and examine their overall and disease-free survival.
Methods
Patients newly diagnosed with CRC in 2003–2005 and 2008 with a survival of at least 1 year after diagnosis and recorded in the retrospective Eindhoven Cancer Registry were included (n = 579). Follow-up was defined as at least one liver imaging and at least two carcinoembryonic antigen (CEA) measurements. Logistic regression analyses were conducted to assess determinants of follow-up. Proportions of patients undergoing colonoscopy, CEA measurements and liver and chest imaging were calculated. Overall and disease-free survival were calculated.
Results
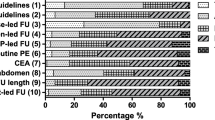
Patients ≥75 years (odds ratio (OR) 0.5 (95% confidence interval (CI) 0.3–0.7)) were less likely to receive follow-up, contrasting patients <50 years (OR 3.1 (95% CI 1.3–7.4)). In 2008, follow-up intensity increased (OR 2.3 (95% CI 1.2–4.3)), especially for liver imaging and CEA measurements. There were large differences in follow-up intensity and activities between hospitals, which were unaffected by comorbidity: ranges for colonoscopy 15–73 %, CEA measurement 46–91 % and imaging of the liver 22–70 % between hospitals. No effect of follow-up intensity was found on 5-year disease-free survival for patients aged <75 years (64 vs. 68 %; p = 0.6). Similarly, no effect of follow-up intensity on 5-year overall survival was found in these patients (77 vs. 82 %; p = 0.07).
Conclusion
Large variation in follow-up was found for patients with CRC, mainly declining with age and hospital of follow-up. Over time, follow-up became more intensive, especially with respect to liver imaging and CEA measurements. However, follow-up consisting of at least one liver imaging and at least two CEA measurements did not improve overall and disease-free survival.




Similar content being viewed by others
References
Comprehensive Cancer Centre Netherlands/Comprehensive Cancer Centre South (2012) www.cijfersoverkanker.nl. Accessed 17 Oct 2012
Manfredi S, Bouvier AM, Lepage C, Hatem C, Dancourt V, Faivre J (2006) Incidence and patterns of recurrence after resection for cure of colonic cancer in a well defined population. Br J Surg 93:1115–1122
National Working Group on Gastrointestinal Cancers (2012) National clinical practice guidelines www.oncoline.nl. Accessed 23 Nov 2012
Tjandra JJ, Chan MK (2007) Follow-up after curative resection of colorectal cancer: a meta-analysis. Dis Colon Rectum 50:1783–1799
Renehan AG, Egger M, Saunders MP, O’Dwyer ST (2002) Impact on survival of intensive follow up after curative resection for colorectal cancer: systematic review and meta-analysis of randomised trials. BMJ 324:1–8
Kievit J (2002) Follow-up of patients with colorectal cancer: numbers needed to test and treat. Eur J Cancer 38:986–999
Jeffery M, Hickey BE, Hider PN (2007) Follow-up strategies for patients treated for non-metastatic colorectal cancer. Cochrane Database Syst Rev CD002200
Bruinvels DJ, Stiggelbout AM, Kievit J, van Houwelingen HC, Habbema JD, van de Velde CJ (1994) Follow-up of patients with colorectal cancer. A meta-analysis. Ann Surg 219:174–182
Figueredo A, Rumble RB, Maroun J, Earle CC, Cummings B, McLeod R, Zuraw L, Zwaal C (2003) Follow-up of patients with curatively resected colorectal cancer: a practice guideline. BMC Cancer 3:26
Rex DK, Kahi CJ, Levin B, Smith RA, Bond JH, Brooks D, Burt RW, Byers T, Fletcher RH, Hyman N, Johnson D, Kirk L, Lieberman DA, Levin TR, O’Brien MJ, Simmang C, Thorson AG, Winawer SJ (2006) Guidelines for colonoscopy surveillance after cancer resection: a consensus update by the American Cancer Society and the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology 130:1865–1871
Janssen-Heijnen MLG, Louwman WJ, van de Poll-Franse LV, Coebergh JWW (2005) Results of 50 years cancer registry in the South of the Netherlands: 1955–2004 (in Dutch). Eindhoven Cancer Registry, Eindhoven
Janssen-Heijnen ML, Houterman S, Lemmens VE, Louwman MW, Maas HA, Coebergh JW (2005) Prognostic impact of increasing age and co-morbidity in cancer patients: a population-based approach. Crit Rev Oncol Hematol 55:231–240
van Duijn C, Keij I (2002) Sociaal-economische status indicator op postcode niveau. Maandstatistiek van de bevolking 50:32–35
Schouten LJ, Hoppener P, van den Brandt PA, Knottnerus JA, Jager JJ (1993) Completeness of cancer registration in Limburg, the Netherlands. Int J Epidemiol 22:369–376
Fritz A, Percy C, Jack A, Shanmugaratnam K, Sobin L, Parkin D, Whelan S (2000) Book international classification of diseases for oncology. World Health Organisation, Geneva
Cardella J, Coburn NG, Gagliardi A, Maier BA, Greco E, Last L, Smith AJ, Law C, Wright F (2008) Compliance, attitudes and barriers to post-operative colorectal cancer follow-up. J Eval Clin Pract 14:407–415
Cooper GS, Yuan Z, Chak A, Rimm AA (1999) Geographic and patient variation among Medicare beneficiaries in the use of follow-up testing after surgery for nonmetastatic colorectal carcinoma. Cancer 85:2124–2131
Korner H, Soreide K, Stokkeland PJ, Soreide JA (2005) Systematic follow-up after curative surgery for colorectal cancer in Norway: a population-based audit of effectiveness, costs, and compliance. J Gastrointest Surg 9:320–328
Grossmann I, de Bock GH, van de Velde CJ, Kievit J, Wiggers T (2007) Results of a national survey among Dutch surgeons treating patients with colorectal carcinoma. Current opinion about follow-up, treatment of metastasis, and reasons to revise follow-up practice. Colorectal Dis 9:787–792
Kievit J (2000) Colorectal cancer follow-up: a reassessment of empirical evidence on effectiveness. Eur J Surg Oncol 26:322–328
Dutch Trial Register (2012) www.trialregister.nl. Accessed 17 Nov 2012
Verberne CJ, Nijboer CH, de Bock GH, Grossmann I, Wiggers T, Havenga K (2012) Evaluation of the use of decision-support software in carcinoembryonic antigen (CEA)-based follow-up of patients with colorectal cancer. BMC Med Inform Decis Mak 12:14
Droz JP, Aapro M, Balducci L (2008) Overcoming challenges associated with chemotherapy treatment in the senior adult population. Crit Rev Oncol Hematol 68(Suppl 1):S1–8
Dutch Health Council (2007) Follow-up in oncology. Identify objectives, substantiate actions. Dutch Health Council, The Hague
van Steenbergen LN, Lemmens VE, Louwman MJ, Straathof JW, Coebergh JW (2009) Increasing incidence and decreasing mortality of colorectal cancer due to marked cohort effects in southern Netherlands. Eur J Cancer Prev 18:145–152
Acknowledgments
The authors thank the registration team of the Eindhoven Cancer Registry for their dedicated data collection. We would like to thank the following hospitals for their cooperation: Amphia Hospital, Jeroen Bosch Hospital, Catharina Hospital Eindhoven, TweeSteden Hospital, VieCuri Medical Centre, Maxima Medical Centre Eindhoven and Veldhoven, Elkerliek Hospital and St Elisabeth Hospital. This study was carried out with a grant from the Dutch Cancer Society (IKZ 2006–3588).
Conflict of interest
The authors have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
van Steenbergen, L.N., de Hingh, I.H.J.T., Rutten, H.J.T. et al. Large variation between hospitals in follow-up for colorectal cancer in southern Netherlands. Int J Colorectal Dis 28, 1257–1265 (2013). https://doi.org/10.1007/s00384-013-1693-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-013-1693-x