Abstract
Purpose
Routine colonic evaluation is advised after an episode of diverticulitis to exclude colorectal cancer. In the recent years, the possible relation between diverticulitis and colorectal cancer has been subject of debate. The aim of this study is to evaluate the benefit of routine colonic endoscopy after an episode of diverticulitis.
Methods
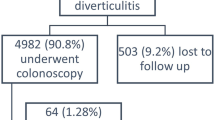
Records of all consecutive patients presenting with a radiologically confirmed episode of diverticulitis between 2007 and 2010 were retrieved from an in-hospital database. Patients who subsequently underwent colonic evaluation were included. The endoscopic detection rate of hyperplastic polyps, adenomas and advanced colonic neoplasia was assessed. Findings were categorized on the basis of the most advanced lesion identified.
Results
Three hundred and seven patients presented with a radiologically confirmed primary episode of diverticulitis. Two hundred and five patients underwent colonic evaluation. Hyperplastic polyps were found in15 (6.8 %), adenomas in 18 (8.8 %) and advanced neoplastic lesions in 7 (3.4 %) patients. Only two patients had a colorectal malignancy.
Conclusion
There appears to be no benefit in performing routine colonic evaluation after an episode of diverticulitis as the incidence of colorectal cancer is almost equal to that of the general population. A more selective approach might therefore be justified. Potentially, only patients with persisting abdominal complaints after an episode of diverticulitis should be offered colonic evaluation to definitively exclude causal pathology.

Similar content being viewed by others
References
Etzioni DA, Mack TM, Beart RW Jr et al (2009) Diverticulitis in the United States: 1998–2005: changing patterns of disease and treatment. Ann Surg 249(2):210–7
Munson KD, Hensien MA, Jacob LN et al (1996) Diverticulitis. A comprehensive follow-up. Dis Colon Rectum 39(3):318–22
Delvaux M (2003) Diverticular disease of the colon in Europe: epidemiology, impact on citizen health and prevention. Aliment Pharmacol Ther 18(Suppl 3):71–4
Sandler RS, Everhart JE, Donowitz M et al (2002) The burden of selected digestive diseases in the United States. Gastroenterology 122(5):1500–11
Mimura T, Emanuel A, Kamm MA (2002) Pathophysiology of diverticular disease. Best Pract Res Clin Gastroenterol 16(4):563–76
Morini S, Hassan C, Zullo A et al (2005) Epithelial cell proliferation of the colonic mucosa in diverticular disease: a case–control study. Aliment Pharmacol Ther 21(11):1385–90
Jacobs DO (2007) Diverticulitis. N Engl J Med 357:2057–66
Rafferty J, Shellito P, Hyman NH et al (2006) Practice parameters for sigmoid diverticulitis. Dis Colon Rectum 49(7):939–44
Westwood DA, Eglinton TW, Frizelle FA (2011) Routine colonoscopy following acute uncomplicated diverticulitis. Br J Surg 98(11):1630–4
Lau KC, Spilsbury K, Farooque Y, Kariyawasam SB, Owen RG, Wallace MH, Makin GB (2011) Is colonoscopy still mandatory after a CT diagnosis of left-sided diverticulitis: can colorectal cancer be confidently excluded? Dis Colon Rectum 54(10):1265–70
Kaiser AM, Jiang JK, Lake JP et al (2005) The management of complicated diverticulitis and the role of computed tomography. Am J Gastronenterol 100:910–917
Lam TJ, Meurs-Szojda MM, Gundlach L, Belien JA, Meijer GA, Mulder CJ, Felt-Bersma RJ (2010) There is no increased risk for colorectal cancer and adenomas in patients with diverticulitis: a retrospective longitudinal study. Colorectal Dis 12(11):1122–6
Niv Y, Hazazi R, Levi Z, Fraser G (2008) Screening colonoscopy for colorectal cancer in asymptomatic people: a meta-analysis. Dig Dis Sci 53(12):3049–54
Bokemeyer B, Bock H, Hüppe D, Düffelmeyer M, Rambow A, Tacke W, Koop H (2009) Screening colonoscopy for colorectal cancer prevention: results from a German online registry on 269000 cases. Eur J Gastroenterol Hepatol 21(6):650–5
Peppas G, Bliziotis IA, Oikonomaki D, Falagas ME (2007) Outcomes after medical and surgical treatment of diverticulitis: a systematic review of the available evidence. J Gastroenterol Hepatol 22(9):1360–8
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
van de Wall, B.J.M., Reuling, E.M.B.P., Consten, E.C.J. et al. Endoscopic evaluation of the colon after an episode of diverticulitis: a call for a more selective approach. Int J Colorectal Dis 27, 1145–1150 (2012). https://doi.org/10.1007/s00384-012-1448-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-012-1448-0