Abstract
Purpose
To quantify the longitudinal division of the internal anal sphincter (IAS) and external anal sphincter (EAS) after fistulotomy using three-dimensional endoanal ultrasound (3D-EAUS) and correlate the results with postoperative faecal incontinence.
Methods
A prospective, consecutive study was performed from December 2008 to October 2010. All patients underwent 3D-EAUS before and 8 weeks after surgery. Thirty-six patients with simple perianal fistula were included. Patients with an intersphincteric or low transphincteric fistula (<66% sphincter involved) without risk factors for incontinence underwent fistulotomy. The outcome measures were the longitudinal extent of division of the IAS and EAS in relation to total sphincter length and continence (Jorge and Wexner scores).
Results
One-year follow-up revealed a 0% recurrence rate. There was a strong correlation between preoperative 3D-EAUS measurement of fistula height with intraoperative and postoperative 3D-EAUS measurement of IAS and EAS division (p < 0.001). The relationship between the level of EAS division and faecal incontinence showed a significant difference in incontinence rates between fistulotomies limited to the lower two thirds of the EAS and those above this level. Five patients (13.9%) had worse anal continence after surgery, although this was mild in all patients (<3/20 Jorge and Wexner scale). There was no significant difference in continence scores before and after surgery (p > 0.05).
Conclusions
In patients without risk factors, division of the EAS during fistulotomy limited to the lower two thirds of the EAS is associated with excellent continence and cure rates.






Similar content being viewed by others
Change history
22 June 2019
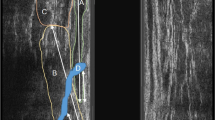
In the Fig. 1 of the original published version of this article the numbers were switched as well as in the text of Results section, lines 5 and 6. The revised figure and the corrected text are now presented correctly in this article.
22 June 2019
In the Fig. 1 of the original published version of this article the numbers were switched as well as in the text of Results section, lines 5 and 6. The revised figure and the corrected text are now presented correctly in this article.
References
Seow-Choen F, Nicholl RJ (1992) Anal Fistula. Br J Surg 79:197–205
Murad-Regadas SM, Regadas FS, Rodrigues LV, Holanda Ede C, Barreto RG, Oliveira L (2010) The role of 3-dimensional anorectal ultrasonography in the assessment of anterior transsphincteric fistula. Dis Colon Rectum 53:1035–1040
Subasinghe D, Samarasekera DN (2010) Comparison of peroperative endoanal ultrasonography with intraoperative findings for fistula in ano. World J Surg 34:1123–1127
Garcés Albir M, García Botello S, Esplapez Valero P et al (2010) Evaluation of three-dimensional endoanal endosonografy of perianal fistulas and correlation with surgical findings. Cir Esp 87:299–305
Santoro GA, Bjorn Fortling EE (2007) The advantages of volume rendering in three-dimensional endosonography of the anorectum. Dis Colon Rectum 50:359–368
Gravante G, Giordano P (2008) The role of three-dimensional endoluminal ultrsound imaging in the evaluation of anorectal disease: a review. Surg Endosc 22:1570–1578
Sboarina A, Miricizzi A, Cordianoc C (2010) New method for internal anal sphincter measurements: feasibility study. Int J Comput Assist Radiol Surg 5:515–525
Roig JV, Jordán J, García-Armengol J et al (2009) Changes in anorectal morphologic and functional parameters after fistula-in-ano surgery. Dis Colon Rectum 52:1462–1469
Jorge JM, Wexner SD (1993) Etiology and management of fecal incontinence. Dis Colon Rectum 36:77–97
Keighley MRB, Williams NS (2008) Fecal icontinence. In: Surgery of the anus, rectum and colon, 3rd edn. Elsevier, Philadelphia, pp 593
Murad-Regadas SM, Regadas FS, Rodrigues LV et al (2011) Anatomic characteristics of anal fistula on three-dimensional anorectal ultrasonography. Dis Colom Rectum 54:460–466
van Koperen PJ, Wind J, Bemelman WA, Bakx R, Reitsma JB, Slors JF (2008) Long-term functional outcomes and risk factors for recurrence after surgical treatment for low and high perianal fistulas of cryptoglandular origin. Dis Colon Rectum 51:1475–1487
Bokhari S, Lindsey I (2010) Incontinence following sphincter division for treatment of anal fistula. Colorectal Dis 12(7 Online):e135–e139
Van der Hagen SJ, Baeten CG, Soeters PB, van Gemert WG (2006) Long-term outcome following mucosal advancement flap for high perianal fistulas and fistulotomy for low perianal fistulas: recurrent perianal fistulas: failure of treatment or recurrent patient disease? Int J Colorectal Dis 21:784–790
Westerterp M, Volkers NA, Poolman RW, van Test WF (2003) Anal fistulotomy between Skylla and Charybdis. Colorectal Dis 5:549–551
Pascual Migueláñez I, García-Olmo D, Martinez-Puente MC, Pascual Montero JA (2005) Is routine endoanal ultrasound useful in anal fistulas? Rev Esp Enferm Dig 97:323–327
Navarro-Luna A, García-Domingo HI, Rius Macias J, Marco-Molina C (2004) Ultrasound study of anal fistulas with hydrogen peroxide enhancement. Dis Colon Rectum 47:108–114
Ratto C, Grillo E, Parello A, Costamagna G, Doglietto GB (2005) Endoanal ultrasound-guided surgery for anal fistula. Endoscopy 37:1–7
Santoro GA, Ratto C, Di Falco G (2004) Three-dimensional reconstruccions improve the accuracy of endoanal ultrasonography in the identification of internal openings of anal fistulas. Colorectal Dis 6(Suppl 2):214
Belmonte Montes C, Ruiz Galindo GH, Montes Villalobos JL, Decanini Terán C (1999) Fistulotomy vs fistulectomy. Ultrasonographic evaluation of lesion of the anal sphincter function. Rev Gastroenterol Mex 64:167–170
Voyvodic F, Rieger NA, Skinner S et al (2003) Endosonographic imaging of anal sphincter injury: does the size of the tear correlate with the degree of dysfunction? Dis Colon Rectum 46:735–741
García-Granero E, Sanahuja A, García-Botello S et al (1998) Anal endosonographic evaluation after closed lateral subcutaneous sphincterotomy. Dis Colon Rectum 41:598–601
García-Granero E, Sanahuja A, García-Botello E et al (2009) The ideal lateral internal sphincterotomy: clinical and endosonographic evaluation following open and closed internal anal sphincterotomy. Colorectal Dis 11:502–507
Sultan AH, Kamm MA, Nicholls RJ, Bartram CI (1994) Prospective study of the extent of internal anal sphincter division during lateral sphincterotomy. Dis Colon Rectum 37:1031–1033
Menteş BB, Ege B, Leventoglu S et al (2005) Extent of lateral internal sphincterotomy: up to the dentate line or up to the fissure apex? Dis Colon Rectum 48:365–370
Menteş BB, Güner MK, Leventoglu S, Akyürek N (2008) Fine-tuning of the extent of lateral internal sphincterotomy: spasm-controlled vs. up to fissure apex. Dis Colon Rectum 51:128–133
Acknowledgements
The manuscript has not received support in the form of grants, equipment, drugs, or all of these. The authors have no relevant financial relationships to disclose. The manuscript was presented as a podium meeting presentation in the 2011 ASCRS Annual Meeting in Vancouver, 14–18 Canada, May.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Garcés-Albir, M., García-Botello, S.A., Esclapez-Valero, P. et al. Quantifying the extent of fistulotomy. How much sphincter can we safely divide? A three-dimensional endosonographic study. Int J Colorectal Dis 27, 1109–1116 (2012). https://doi.org/10.1007/s00384-012-1437-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-012-1437-3