Abstract
Background and aim
The aim of this retrospective study was to determine which clinicopathological factors influenced the incidence of postoperative relapse and overall survival rates after radical resection of T2-4N0M0 colorectal cancer (CRC) patients via harvesting a minimum of 12 lymph nodes.
Materials and methods
Between January 2001 and June 2006, a total of 342 T2-4N0M0 CRC patients who underwent radical resection were retrospectively analyzed in Kaohsiung Medical University Hospital. Of these 342 patients, 155 were observed by harvesting a minimum of 12 lymph nodes. These 155 patients were followed up intensively, and their outcomes were investigated retrospectively.
Results
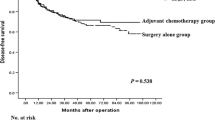
Of 155 patients, 83 were men (53.5%) and 72 (46.5%) were women. The mean age was 65.5 ± 11.1 years (range, 24–89 years). The median follow-up period was 49 months (range, 19–80 months). The present data showed invasive depth (P = 0.012), vascular invasion (P < 0.001), and perineural invasion (P = 0.009) as significantly prognostic factors for postoperative 5-year relapse rate by Kaplan–Meier analysis. Likewise, invasive depth (P = 0.013), vascular invasion (P < 0.001), and perineural invasion (P = 0.008) were significant factors for postoperative 5-year survival rate. Meanwhile, using a Cox proportional hazards analysis, depth of tumor invasion (P = 0.026) and vascular invasion (P = 0.001) were the independent predictors for postoperative relapse. Furthermore, the presence of vascular invasion was considerably correlated to the higher postoperative relapse rate and the poorer overall survival rates by survival analyses (P < 0.0001).
Conclusions
Besides the conventional depth of tumor invasion, this study highlights the potential for using vascular invasion as a means of identifying a subgroup of T2-4N0M0 CRC patients with adequate lymph node harvest at higher risk who would potential benefit from adjuvant therapy after surgery.





Similar content being viewed by others
References
Green FL, Stewart AK, Norton HJ (2002) A new TNM staging strategy for node-positive (stage III) colon cancer: an analysis of 50,042 patients. Am Surg 236:416–421
International Union Against Cancer (eds) (2002) TNM classification of malignant tumors. Wiley-Liss, New York
Hase K, Shatney C, Johnson D, Trollope M, Vierra M (1993) Prognostic value of tumor “budding” in patients with colorectal cancer. Dis Colon Rectum 36:627–635
Tsai HL, Lu CY, Hsieh JS, Wu DC, Jan CM, Chai CY, Chu KS, Chan HM, Wang JY (2007) The prognostic significance of total lymph node harvest in patients with T2-4N0M0 colorectal cancer. J Gastrointest Surg 11:660–665
Field LP, Arsenault PA, Chapuis PH, Dent O, Gathright B, Hardcastle JD, Hermanek P, Jass JR, Newland RC (1991) Clinicopathological staging for colorectal cancer: an International Documentation System (IDS) and an International Comprehensive Anatomical Terminology (ICAT). J Gastroenterol Hepatol 6:325–344
Merkel S, Wein A, Gunther K, Papadopoulos T, Hohenberger W, Hermanek P (2001) High-risk groups of patients with stage II colon carcinoma. Cancer 92:1435–1443
Davis NC, Newland RC (1983) Terminology and classification of colorectal adenocarcinoma: the Australian clinicopathological staging system. Aust N Z J Surg 53:211–221
Mulcahy HE, Toner M, Patchett SE, Daly L, O’Donoghue DP (1997) Identifying stage B colorectal patients at high risk of tumor recurrence and death. Dis Colon Rectum 40:326–331
Nelson H, Petrelli N, Carlin A, Couture J, Fleshman J, Guillem J, Miedema B, Ota D, Sargent D (2001) Guidelines 2000 for colon and rectal cancer surgery. J Natl Cancer Inst 93:583–596
Fujita S, Shimoda T, Yoshimura K, Yamamoto S, Akasu T, Moriya Y (2003) Prospective evaluation of prognostic factors in patients with colorectal cancer undergoing curative resection. J Surg Oncol 84:127–131
Krasna MJ, Flancbaum L, Cody RP, Shneibaum S, Ben Ari G (1988) Vascular and neural invasion in colorectal carcinoma: incidence and prognostic significance. Cancer 61:1018–1023
Horn A, Dahl O, Morild I (1991) Venous and neural invasion as predictors of recurrence in rectal adenocarcinoma. Dis Colon Rectum 34:798–804
Bayar S, Saxena R, Emir B, Salem RR (2002) Venous invasion may predict lymph node metastasis in early rectal cancer. Eur J Surg Oncol 28:413–417
Meguerditchian AN, Bairati I, Lagace R, Harel F, Kibrite A (2005) Prognostic significance of lymphovascular invasion in surgically cured rectal carcinoma. Am J Surg 189:707–713
Shirouzu K, Isomoto H, Kakegawa T, Morimatsu M (1991) A prospective clinicopathologic study of venous invasion in colorectal cancer. Am J Surg 162:216–222
Inoue T, Mori M, Shimono R, Kuwano H, Sugimachi K (1992) Vascular invasion of colorectal carcinoma readily visible with certain stains. Dis Colon Rectum 35:34–39
Ouchi K, Sugawara T, Ono H, Fujiya T, Kamiyama Y, Kakugawa Y, Mikuni J, Tateno H (1996) Histologic features and clinical significance of venous invasion in colorectal carcinoma with hepatic metastasis. Cancer 78:2313–2317
Tsuchiya A, Ando Y, Kikuchi Y, Kanazawa M, Sato H, Abe R (1995) Venous invasion as a prognostic factor in colorectal cancer. Surg Today 25:950–953
Minsky BD, Mies C, Recht A, Rich TA, Chaffey JT (1998) Resectable adenocarcinoma of the rectosigmoid and rectum: the influence of blood vessel invasion. Cancer 61:1417–1424
Khanlhanian N, Mavligit GM, Russell WO, Schimek M (1997) Prognostic significance of vascular invasion in colorectal cancer of Dukes’ B class. Cancer 39:1195–1200
Ptok H, Meyer F, Steinert R, Vieth M, Ridwelski K, Lipper H, Gastinger I (2007) No prognostic impact isolated lymphovascular invasion after radical resection of rectal cancer—results of a multicenter observation study. Int J Colorectal Dis 22:749
Seefeld PH, Bargen JA (1943) The spread of carcinoma of the rectum, invasion of the lymphatic system, veins and nerves. Ann Surg 118:76–90
Ueno H, Hase K, Mochizuki H (2001) Criteria for extramural perineural invasion as a prognostic factor in rectal cancer. Br J Surg 88:994–1000
Bruinvels DJ, Stiggelbout AM, Kievit J, van Houwelingen HC, Habbema JD, van de Velde CJ (1994) Follow-up pf patients with colorectal cancer. A meta-analysis. Ann Surg 219:174–182
Acknowledgment
The authors would like to thank Yang Yi-Sing (Statistical Analysis Laboratory, Department of Medical Research, Kaohsiung Medical University Hospital) for her assistance of the statistical analysis. We also sincerely thank Drs. Deng-Chyang Wu, Hon-Man Chan, Che-Jen Huang, and Jan-Sing Hsieh for having contributed materially to the paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tsai, HL., Yeh, YS., Yu, FJ. et al. Predicting factors of postoperative relapse in T2-4N0M0 colorectal cancer patients via harvesting a minimum of 12 lymph nodes. Int J Colorectal Dis 24, 177–183 (2009). https://doi.org/10.1007/s00384-008-0594-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-008-0594-x