Abstract
Purpose
Very low birth weight infants (VLBWIs) have been thought as risk of bad outcomes in the patients with esophageal atresia (EA). However, detailed outcomes of EA within VLBWIs were not fully understood. We aimed to reveal short- and long-term outcomes in VLBWIs with EA.
Methods
Clinical data regarding VLBWIs with EA registered in Neonatal Research Network Japan, a multicenter research database in Japan, were collected. Patients with chromosomal abnormality were excluded. Short term outcome was survival discharge from NICU and long-term outcome was neurodevelopmental impairment (NDI) at 3 years.
Results
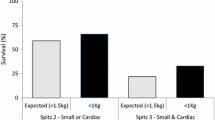
A total of 103 patients were analyzed. the overall survival discharge rate from NICU was 68.0% (70/103). The risk of death was increased as the birth weight got reduced. The presence of associated anomaly increased the risk of death. Three-year neurodevelopmental information was available in 32.9% (23/70) of patients. Of the 23 included patients for 3-year follow-up, 34.8% had NDI. The risk of NDI was increased as the birth weight reduced.
Conclusions
In VLBWIs with EA, survival discharge from NICU was still not high. More immature patients and patients with an associated anomaly had worse outcomes. Among patients who survived, NDI was confirmed in a certain number of patients.



Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author, H.M., upon reasonable request.
References
Spitz L (2006) Esophageal atresia. Lessons I have learned in a 40-year experience. J Pediatr Surg 41:1635–1640
Holcomb III GW (2010). In: Murphy JP (ed) Ashcraft’s pediatric surgery, fifth. Saunders
Gross RE, Ladd WE (1953) The Surgery of infancy and childhood: its principles and techniques. WB Saunders, Philadelphia and London
Spitz L (1996) Esophageal atresia: past, present, and future. J Pediatr Surg 31:19–25
Spitz L, Kiely EM, Morecroft JA et al (1994) Oesophageal atresia: at-risk groups for the 1990s. J Pediatr Surg 29:723–725
Malakounides G, Lyon P, Cross K et al (2016) Esophageal atresia: improved outcome in high-risk groups revisited. Eur J Pediatr Surg 26:227–231
Ludman L, Spitz L, Lansdown R (1993) Intellectual development at 3 year of age of age of children who underwent major neonatak Surgery. J Pediatr Surg 28:130–134
Kubota A, Nose K, Yamamoto E et al (2011) Psychosocial and cognitive consequences of major neonatal Surgery. J Pediatr Surg 46:2250–2253
Kubota A, Yamakawa S, Yamamoto E et al (2016) Major neonatal Surgery: psychosocial consequence of the patients and mothers. J Pediatr Surg 51:264–267
Stolwijk LJ, Lemmers PM, Harmsen M et al (2016) Neurodevelopmental outcomes after neonatal surgery for major noncardiac anomalies. Pediatrics 137:e20151728
Ijsselstijn H, Gischler S, Toussaint L et al (2016) Growth and development after oesophageal atresia surgery: need for long-term multidisciplinary follow-up. Pediatr Res Rev 19:34–38
Okuyama H, Tazuke Y, Ueno T et al (2017) Long-term morbidity in adolescents and young adults with surgically treated esophageal atresia. Surg Today 47:872–876
Roorda D, Konigs M, Eeftnick Schattenkerk L et al (2021) Neurodevelopmental outcome of patients with congenital gastrointestinal malformations: a systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed 106:F635–642
Kono Y, on behalf of the Neonatal Research Network of Japan (2021) Neurodevelopmental outcomes of very low birth weight infants in the Neonatal Research Network of Japan: importance of neonatal intensive care unit graduate follow-up. Clin Exp Pediatr 64:313–321
Kusuda S, Fujimura M, Sakuma I et al (2006) Neonatal Research Network, Japan morbidity and mortality of infants with very low birth weight in Japan: center variation. Pediatrics 118:e1130-1138
Kono Y, Mishima J, Yonemoto N et al (2011) Outcomes of very-low-birthweight infants at 3 years of age born in 2003–2004 in Japan. Pediatr Int 53:1051–1058
The Japan Neonatal Follow-up Study Group. Protocol for the multicenter follow-up study of VLBW infants (in Japanese). http://highrisk-followup.jp/schedule/. Accessed 4 Aug 2023
Palisano R, Rosenbaum P, Walter S et al (1997) Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol 39:214–223
Society for the Kyoto Scale of psychological development test (2008) Simpan K Shiki Hattatsu Kensahou 2001 (in Japanese). Nakanishiya Shuppan
Kono Y, Yonemoto N, Kusuda S et al (2016) Developmental assessment of VLBW infants at 18 months of age: a comparison study between KSPD and Bayley III. Brain Dev 38:377–385
e-Stat : Statistics of Japan: https://www.e-stat.go.jp/dbview?sid=0003411614 . Accessed 4 Aug 2023
Kusuda S, Fujimura M, Uchiyama A et al (2012) Trends in morbidity and mortality among very-low-birth-weight infants from 2003 to 2008 in Japan. Ped Res 72:531–538
Nishi E, Takamizawa S, Iio K et al (2014) Surgical intervention for esophageal atresia in patients with trisomy 18. Am J Med Genet Part A 164A:324–330
Springett A, Wellesley D, Greenlees R et al (2015) Congenital anomalies associated with trisomy 18 or trisomy 13: a geristry-based study in 16 European countries, 2000–2011. Am J Med Genet Part A 167A:3062–3069
Iida C, Muneuchi J, Yamamoto J et al (2020) Impacts of surgical interventions on the long-term outcomes in individuals with trisomy 18. J Pediatr Surg 55:2466–2470
Keefe G, Culbreath K, Edwards EM et al (2022) Current outcomes of infants with esophageal atresia and tracheoesophageal fistula: a multicenter analysis. J Pediatr Surg 57:970–974
Schmidt A, Obermayr F, Lieber J et al (2017) Outcome of primary repair I extremely and very low-birth-weight infants with esophageal atresia/distal tracheoesophageal fistula. J Pediatr Surg 52:1567–1570
Oztan MO, Soyer T, Oztorun CI et al (2021) Outcome of very low and low birth weight infants with esophageal atresia: results of the Turkish esophageal atresia registry. Eur J Pediatr Surg 31:226–235
Sfeir R, Rousseau V, Bonnard A et al (2021) Risk factors of early mortality and morbidity in esophageal atresia with distal tracheoesophageal fistula: a population-based cohort study. J Pediatr 234:99–105
Koivusalo AI, Suominen JS, Pakarinen MP (2022) Oesophageal atresia with very low birth weight: clinical characteristics and long-term outcome. J Pediatr Surg 57:192–194
Walden RV, Taylor SC, Hansen NI et al (2007) Major congenital anomalies place extremely low birth weight infants at higher risk for poor growth and developmental outcomes. Pediatrics 120:e1512
Acknowledgements
The authors appreciate members of the Neonatal Research Network of Japan, and the investigators of the participating institutions.
Author information
Authors and Affiliations
Consortia
Contributions
HM and HS designed the study. HM and SY collected and analyzed data. HM wrote the main manuscript. RN and TI contributed to refine study concept and design. All authors critically reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Miyake, H., Nakano, R., Yamamoto, S. et al. Mortality and neurodevelopmental outcomes in very low birth weight infants with esophageal atresia. Pediatr Surg Int 39, 294 (2023). https://doi.org/10.1007/s00383-023-05579-8
Accepted:
Published:
DOI: https://doi.org/10.1007/s00383-023-05579-8