Abstract
Purpose
Children with Hirschsprung’s disease (HD) and anorectal malformations (ARM) may benefit from a bowel management program (BMP) to treat constipation and fecal incontinence. This study describes a pilot BMP in Uganda.
Methods
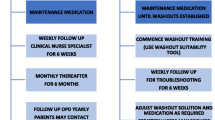
Patients treated for HD or ARM were recruited for the BMP. Local staff underwent training and progressively took over decision-making. The rates of patient involuntary bowel movements (IBMs) and provider confidence were evaluated pre- and post-BMP with questionnaires. The results were compared with Fischer’s exact test.
Results
Ten staff—2 surgeons, 6 nurses and 2 physiotherapists—and 12 patients participated. Patient median age was 4.5 years (IQR 3–6.6) and ten were male. Ten reported at least daily IBMs prior to the BMP. All patients underwent a clean-out. The parents were then taught to perform daily enemas or irrigations. Specific regimens were determined by patient history and imaging and titrated throughout the BMP. There were differences in the rates of both daytime and nighttime IBMs before and after the BMP (p = 0.0001 and 0.002, respectively). All staff reported increased confidence.
Conclusions
We describe the first BMP in Uganda. BMPs can successfully treat constipation and fecal incontinence in low-income countries, although there are challenges with resources and follow-up.




Similar content being viewed by others
Data availability
Sample teaching resources and survey tools have been made available in the supplemental files. Given the small sample size and concerns about patient confidentiality, individual patient data is not available.
References
Peña A, Guardino K, Tovilla JM, Levitt MA, Rodriguez G, Torres R (1998) Bowel management for fecal incontinence in patients with anorectal malformations. J Pediatr Surg 33(1):133–137
Bischoff A, Levitt MA, Peña A (2009) Bowel management for the treatment of pediatric fecal incontinence. Pediatr Surg Int 25(12):1027–1042
Levitt MA, Martin CA, Olesevich M, Bauer CL, Jackson LE, Peña A (2009) Hirschsprung disease and fecal incontinence: diagnostic and management strategies. J Pediatr Surg 44(1):271–277 (discussion 7)
Levitt MA, Peña A (2010) Pediatric fecal incontinence: a surgeon’s perspective. Pediatr Rev 31(3):91–101
Lim IIP, Cushing CC, Jenkins T, Troutt M, Zeller MH, Hossain M et al (2021) Prospective quality of life outcomes in pediatric fecal incontinence following bowel management. J Pediatr Surg 56(8):1459–1464
Wood RJ, Vilanova-Sanchez A, El-Gohary Y, Ahmad H, Halleran DR, Reck-Burneo CA et al (2021) One-year impact of a bowel management program in treating fecal incontinence in patients with anorectal malformations. J Pediatr Surg 56(10):1689–1693
Colares JH, Purcaru M, da Silva GP, Frota MA, da Silva CA, Melo-Filho AA et al (2016) Impact of the bowel management program on the quality of life in children with fecal incontinence. Pediatr Surg Int 32(5):471–476
Kilpatrick JA, Zobell S, Leeflang EJ, Cao D, Mammen L, Rollins MD (2020) Intermediate and long-term outcomes of a bowel management program for children with severe constipation or fecal incontinence. J Pediatr Surg 55(3):545–548
Wang Y, Liang H, Wu Q, Zheng H, Liu G, Wen Z et al (2017) Bowel management program for pediatric postoperative fecal incontinence in China: a surgeon’s experience. Medicine (Baltimore) 96(22):e7078
Gabr AA, Gad MA, Shalaby A (2020) Quality of life in children with pseudoincontinence after implementing a bowel management program in Egypt. J Pediatr Surg 55(2):261–264
Shahba Z, Ahmadi B, Haji Bandeh S, Hosseinpour M (2022) Evaluation of bowel management program on quality of life in children with fecal incontinence. Adv Biomed Res 11:69
The World Bank, World Development Indicators (2022). The World by Income [Data file]. Retrieved from https://datatopics.worldbank.org/world-development-indicators/the-world-by-income-and-region.html Accessed 19 Sept 2023
Oyania F, Ogwal A, Nimanya S, Muzira A, Kakembo N, Kisa P et al (2020) Long term bowel function after repair of anorectal malformations in Uganda. J Pediatr Surg 55(7):1400–1404
Pilkington M, Situma M, Winthrop A, Poenaru D (2018) Quantifying delays and self-identified barriers to timely access to pediatric surgery at Mbarara Regional Referral Hospital. Uganda J Pediatr Surg 53(5):1073–1079
Kayima P, Kitya D, Punchak M, Anderson GA, Situma M (2019) Patterns and treatment outcomes of anorectal malformations in Mbarara Regional Referral Hospital. Uganda J Pediatr Surg 54(4):838–844
Trinidad S, Kayima P, Kotecha V, Massenga A, Rymeski B, Frischer JS et al (2022) Hirschsprung’s disease in low- and middle-income countries. Semin Pediatr Surg 31(2):151163
Ekenze SO, Ngaikedi C, Obasi AA (2011) Problems and outcome of Hirschsprung’s disease presenting after 1 year of age in a developing country. World J Surg 35(1):22–26
Muzira A, Kakembo N, Kisa P, Langer M, Sekabira J, Ozgediz D et al (2018) The socioeconomic impact of a pediatric ostomy in Uganda: a pilot study. Pediatr Surg Int 34(4):457–466
Author information
Authors and Affiliations
Contributions
Study conception and design: ST, FO, MO, MK, and MS. Acquisition of data: ST, FO, CB, IN, MO, CO, and MK. Analysis and interpretation of data: ST, FO, CB, IN, MO, CO, and MK. Drafting of manuscript: ST. Critical revision of manuscript: FO, CO, and MK.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Trinidad, S., Oyania, F., Bingana, C. et al. Pilot bowel management program at Mbarara Hospital, Uganda. Pediatr Surg Int 39, 292 (2023). https://doi.org/10.1007/s00383-023-05574-z
Accepted:
Published:
DOI: https://doi.org/10.1007/s00383-023-05574-z