Abstract
Purpose
Postoperative anastomotic stricture (PAS) is a well-known complication after correcting choledochal cyst (CC). Although the exact cause of PAS is unknown, various risk factors, such as Todani classification type IV-A, hepaticoduodenostomy, and narrow anastomosis have been reported to be associated with PAS. As far as we know, there is no report with a cumulative analysis of such risk factors of PAS. This systematic review and meta-analysis aimed to investigate the risk factors of PAS following surgical correction of CC in children.
Methods
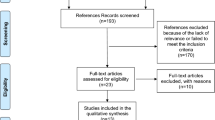
A systematic literature search for relevant articles was performed in four databases using the combinations of the following terms “Congenital biliary dilatation”, “Congenital choledochal cyst”, “Choledochal cyst”, “Stenosis”, “Stricture”, and “Complication” for studies published between 1973 and 2022. The relevant cohorts of PAS were systematically searched for clinical presentation and outcomes.
Results
The search strategy identified 795 reports. Seventy studies met the defined inclusion criteria, reporting a total of 206 patients with PAS. There is no prospective study in this search. The incidence of PAS was 2.1%. The proportion of Todani classification of the patient with PAS was higher in type IV-A with significant difference (2.0% in type I and 10.1% in type IV-A (p = 0.001)). Fourteen studies reported a comparison between hepaticojejunostomy and hepaticoduodenostomy. There was no significant difference between the two groups (p = 0.36). Four studies reported the diameter of the anastomosis at the primary surgery. The mean diameter was 12.5 mm. Nine studies reported a comparison between laparoscopic surgery and open surgery. Pooled odds ratio of PAS did not show a statistical difference (p = 0.29).
Conclusions
This study suggests that close careful follow-up is important in the patients with type IV-A of CC who underwent excision surgery, considering the possibility of PAS.




Similar content being viewed by others
References
Hyvärinen I, Hukkinen M, Kivisaari R et al (2021) Long-term morbidity of choledochal malformations in children. J Pediatr Gastroenterol Nutr 72:820–825
Shimotakahara A, Yamataka A, Kobayashi H et al (2003) Forme fruste choledochal cyst: long-term follow-up with special reference to surgical technique. J Pediatr Surg 38:1833–1836
Todani T, Watanabe Y, Toki A et al (1998) Co-existing biliary anomalies and anatomical variants in choledochal cyst. Br J Surg 85:760–763
Ishibashi H, Shimada M, Kamisawa T et al (2017) Japanese clinical practice guidelines for congenital biliary dilatation. J Hepatobiliary Pancreat Sci 24:1–16
Kim JH, Choi TY, Han JH et al (2008) Risk factors of postoperative anastomotic stricture after excision of choledochal cysts with hepaticojejunostomy. J Gastrointest Surg 12:822–828
Todani T, Watanabe Y, Toki A et al (1988) Reoperation for congenital choledochal cyst. Ann Surg 207:142–147
Xie X, Li K, Wang J et al (2020) Comparison of pediatric choledochal cyst excisions with open procedures, laparoscopic procedures and robot-assisted procedures: a retrospective study. Surg Endosc 34:3223–3231
Miyano T, Yamataka A, Kato Y et al (1996) Hepaticoenterostomy after excision of choledochal cyst in children: a 30-year experience with 180 cases. J Pediatr Surg 31:1417–1421
Page MJ, Moher D, Bossuyt PM et al (2021) PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ 372:n160
Amano H, Shirota C, Tainaka T et al (2021) Late postoperative complications of congenital biliary dilatation in pediatric patients: a single-center experience of managing complications for over 20 years. Surg Today 51:1488–1495
Tainaka T, Shirota C, Hinoki A et al (2022) Laparoscopic definitive surgery for congenital biliary dilatation with aggressive hilar bile ductoplasty and complete resection of the intrapancreatic bile duct in pediatric patients is safe and effective, comparable to open surgery. Surg Endosc 36:7352–7359
Qiao G, Li L, Li S et al (2015) Laparoscopic cyst excision and Roux-Y hepaticojejunostomy for children with choledochal cysts in China: a multicenter study. Surg Endosc 29:140–144
Alizai NK, Dawrant MJ, Najmaldin AS (2014) Robot-assisted resection of choledochal cysts and hepaticojejunostomy in children. Pediatr Surg Int 30:291–294
Chang EY, Hong YJ, Chang HK et al (2012) Lessons and tips from the experience of pediatric robotic choledochal cyst resection. J Laparoendosc Adv Surg Tech A 22:609–614
Dalton BG, Gonzalez KW, Dehmer JJ et al (2016) Transition of techniques to treat choledochal cysts in children. J Laparoendosc Adv Surg Tech A 26:62–65
Hamada Y, Hamada H, Shirai T et al (2017) Duodenogastric regurgitation in hepaticoduodenostomy after excision of congenital biliary dilatation (choledochal cyst). J Pediatr Surg 52:1621–1624
Yeung F, Fung ACH, Chung PHY et al (2020) Short-term and long-term outcomes after Roux-en-Y hepaticojejunostomy versus hepaticoduodenostomy following laparoscopic excision of choledochal cyst in children. Surg Endosc 34:2172–2177
Mukhopadhyay B, Shukla RM, Mukhopadhyay M et al (2011) Choledochal cyst: a review of 79 cases and the role of hepaticodochoduodenostomy. J Indian Assoc Pediatr Surg 16:54–57
Ono S, Maeda K, Baba K et al (2013) The efficacy of double-balloon enteroscopy for intrahepatic bile duct stones after Roux-en-Y hepaticojejunostomy for choledochal cysts. Pediatr Surg Int 29:1103–1107
Yu BH, Lin F (2016) Clinical effects in resection of congenital choledochal cyst of children and jejunum Roux-Y anastomosis by laparoscope. Eur Rev Med Pharmacol Sci 20:4530–4534
Zhuansun D, Jiao C, Meng X et al (2020) A study of three-dimensional versus two-dimensional laparoscopic surgery in resection of congenital choledochal cyst of children and jejunum Roux-en-Y anastomosis. J Laparoendosc Adv Surg Tech A 30:344–349
Hata Y, Sasaki F, Takahashi H et al (1993) Surgical treatment of congenital biliary dilatation associated with pancreaticobiliary maljunction. Surg Gynecol Obstet 176:581–587
Saing H, Han H, Chan KL et al (1997) Early and late results of excision of choledochal cysts. J Pediatr Surg 32:1563–1566
Watanabe Y, Toki A, Todani T (1999) Bile duct cancer developed after cyst excision for choledochal cyst. J Hepatobiliary Pancreat Surg 6:207–212
Yamataka A, Ohshiro K, Okada Y et al (1997) Complications after cyst excision with hepaticoenterostomy for choledochal cysts and their surgical management in children versus adults. J Pediatr Surg 32:1097–1102
Nakamura T, Okada A, Higaki J et al (1996) Pancreaticobiliary maljunction-associated pancreatitis: an experimental study on the activation of pancreatic phospholipase A2. World J Surg 20:543–550
Diao M, Li L, Cheng W (2011) Laparoscopic versus Open Roux-en-Y hepatojejunostomy for children with choledochal cysts: intermediate-term follow-up results. Surg Endosc 25:1567–1573
Diao M, Li L, Cheng W (2016) Laparoscopic redo hepaticojejunostomy for children with choledochal cysts. Surg Endosc 30:5513–5519
Foo DC, Wong KK, Lan LC et al (2009) Impact of prenatal diagnosis on choledochal cysts and the benefits of early excision. J Paediatr Child Health 45:28–30
Gardikis S, Antypas S, Kambouri K et al (2005) The Roux-en-Y procedure in congenital hepato-biliary disorders. Rom J Gastroenterol 14:135–140
Guan X, Li J, Wang Z et al (2022) Timing of operation in children with a prenatal diagnosis of choledochal cyst: a single-center retrospective study. J Hepatobiliary Pancreat Sci. https://doi.org/10.1002/jhbp.1155
Li S, Wang W, Yu Z et al (2014) Laparoscopically assisted extrahepatic bile duct excision with ductoplasty and a widened hepaticojejunostomy for complicated hepatobiliary dilatation. Pediatr Surg Int 30:593–598
Miyake H, Fukumoto K, Yamoto M et al (2022) Pancreaticobiliary maljunction without biliary dilatation in pediatric patients. Surg Today 52:207–214
Ohyama K, Furuta S, Shima H et al (2021) Differences in post-operative complications after reconstruction for congenital biliary dilatation in a single institution-Roux-en-Y hepaticojejunostomy versus hepaticoduodenostomy. Pediatr Surg Int 37:241–245
Zhang B, Wu D, Fang Y et al (2019) Early complications after laparoscopic resection of choledochal cyst. Pediatr Surg Int 35:845–852
Nederlandse Studiegroep voor Choledochus Cm, van den Eijnden MHA, de Kleine RHJ et al (2017) Choledochal malformation in children: lessons learned from a dutch national study. World J Surg 41:2631–2637
Santore MT, Behar BJ, Blinman TA et al (2011) Hepaticoduodenostomy vs hepaticojejunostomy for reconstruction after resection of choledochal cyst. J Pediatr Surg 46:209–213
She WH, Chung HY, Lan LC et al (2009) Management of choledochal cyst: 30 years of experience and results in a single center. J Pediatr Surg 44:2307–2311
Todani T, Watanabe Y, Urushihara N et al (1995) Biliary complications after excisional procedure for choledochal cyst. J Pediatr Surg 30:478–481
Liem NT, Pham HD, Dung LA et al (2012) Early and intermediate outcomes of laparoscopic surgery for choledochal cysts with 400 patients. J Laparoendosc Adv Surg Tech A 22:599–603
Ohi R, Yaoita S, Kamiyama T et al (1990) Surgical treatment of congenital dilatation of the bile duct with special reference to late complications after total excisional operation. J Pediatr Surg 25:613–617
Redkar R, Davenport M, Howard ER (1998) Antenatal diagnosis of congenital anomalies of the biliary tract. J Pediatr Surg 33:700–704
Urushihara N, Fukumoto K, Fukuzawa H et al (2012) Long-term outcomes after excision of choledochal cysts in a single institution: operative procedures and late complications. J Pediatr Surg 47:2169–2174
Chi S-q, Cao G-q, Li S et al (2021) Outcomes in robotic versus laparoscopic-assisted choledochal cyst excision and hepaticojejunostomy in children. Surg Endosc 35:5009–5014
Kim NY, Chang EY, Hong YJ et al (2015) Retrospective assessment of the validity of robotic surgery in comparison to open surgery for pediatric choledochal cyst. Yonsei Med J 56:737–743
Lin S, Chen J, Tang K et al (2022) Trans-umbilical single-site plus one robotic assisted surgery for choledochal cyst in children, a comparing to laparoscope-assisted procedure. Front Pediatr 10:806919
Senthilnathan P, Patel ND, Nair AS et al (2015) Laparoscopic management of choledochal cyst-technical modifications and outcome analysis. World J Surg 39:2550–2556
Son TN, Liem NT, Hoan VX (2014) Transumbilical laparoendoscopic single-site surgery with conventional instruments for choledochal cyst in children: early results of 86 cases. J Laparoendosc Adv Surg Tech A 24:907–910
Tang ST, Yang Y, Wang Y et al (2011) Laparoscopic choledochal cyst excision, hepaticojejunostomy, and extracorporeal Roux-en-Y anastomosis: a technical skill and intermediate-term report in 62 cases. Surg Endosc 25:416–422
Zheng J, Li Z, Ye Y et al (2020) Short-term complications after laparoscopic choledochal cyst radical surgery: prevention and treatment. Front Surg 7:583210
Oweida SW, Ricketts RR (1989) Hepatico-jejuno-duodenostomy reconstruction following excision of choledochal cysts in children. Am Surg 55:2–6
Chijiiwa K (1993) Hazard and outcome of retreated choledochal cyst patients. Int Surg 78:204–207
Uno K, Tsuchida Y, Kawarasaki H et al (1996) Development of intrahepatic cholelithiasis long after primary excision of choledochal cysts. J Am Coll Surg 183:583–588
Cosentino CM, Luck SR, Raffensperger JG et al (1992) Choledochal duct cyst: resection with physiologic reconstruction. Surgery 112:740–747 (discussion 747-748)
Acker SN, Bruny JL, Narkewicz MR et al (2013) Preoperative imaging does not predict intrahepatic involvement in choledochal cysts. J Pediatr Surg 48:2378–2382
Barlow B, Tabor E, Blanc WA et al (1976) Choledochal cyst: a review of 19 cases. J Pediatr 89:934–940
Diao M, Li L, Cheng W (2016) Recurrence of biliary tract obstructions after primary laparoscopic hepaticojejunostomy in children with choledochal cysts. Surg Endosc 30:3910–3915
Fu M, Wang Y, Zhang J (2000) Evolution in the treatment of choledochus cyst. J Pediatr Surg 35:1344–1347
Germani M, Liberto D, Elmo G et al (2011) Choledochal cyst in pediatric patients: a 10-year single institution experience. Acta Gastroenterol Latinoam 41:302–307
Hamada Y, Sato M, Takada K et al (1998) Spiral computed tomography for bilioenteric anastomotic stricture. Pediatr Surg Int 13:424–425
Joseph VT (1990) Surgical techniques and long-term results in the treatment of choledochal cyst. J Pediatr Surg 25:782–787
Kim JW, Moon SH, Park DH et al (2010) Course of choledochal cysts according to the type of treatment. Scand J Gastroenterol 45:739–745
Lilly JR, Stellin GP, Karrer FM (1985) Forme fruste choledochal cyst. J Pediatr Surg 20:449–451
Miyano T, Suruga K, Chen SC (1980) A clinicopathologic study of choledochal cyst. World J Surg 4:231–238
Miyano G, Koyama M, Miyake H et al (2017) Comparison of laparoscopic hepaticojejunostomy and open hepaticojejunostomy. Can stenosis of the hilar hepatic duct affect postoperative outcome? Asian J Endosc Surg 10:295–300
Saing H, Chan KL, Mya GH et al (1996) Cutaneous stoma in the roux limb of hepaticojejunostomy (hepaticocutaneous jejunostomy): useful access for intrahepatic stone extraction. J Pediatr Surg 31:247–250
Saing H, Chan JK, Lam WW et al (1998) Virtual intraluminal endoscopy: a new method for evaluation and management of choledochal cyst. J Pediatr Surg 33:1686–1689
Sheng Q, Lv Z, Xu W et al (2017) Reoperation after cyst excision with hepaticojejunostomy for choledochal cysts: our experience in 18 cases. Med Sci Monit 23:1371–1377
Yeung F, Chung PH, Wong KK et al (2015) Biliary-enteric reconstruction with hepaticoduodenostomy following laparoscopic excision of choledochal cyst is associated with better postoperative outcomes: a single-centre experience. Pediatr Surg Int 31:149–153
Hamada Y, Sato M, Uetuji S (1992) Initial surgical technique for congenital dilatation of the biliary tract—a study from reoperation cases-(Japanese). J Jpn Surg Assoc 53:2631–2637
Kamiyama T, Ohi R, Hayashi Y (1994) Late complications of congenital dilatation of the bile duct-with special reference to intrahepatic gallstones after hepatico-jejunostomy-(Japasene). J Jpn Soc Pediatr Surg 30:1069–1074
Kidogawa H, Ito S, Yamayoshi T et al (2009) A case of left hepatectomy for left hepaticojejunostomy stricture after operation for congenital bile duct dilatation (Japanese). Jpn J Gastroenterol Surg 42:1402–1406
Kubota A, Kawahara H, Okuyama T et al (2004) Clinical outcome after biliary reconstruction for pancreaticobiliary maljunction (Japanese). Jpn J Pediatr Surg 36:501–506
Todani T, Watanabe T, Uemura S (1992) Pathophysiology and treatment of benign bile duct stricture (Japanese). J Biliary Tract and Pancr 13:1191–1195
Miyano T (1973) The clinical and pathological study of the congenital dilatation of the common bile duct. J Jpn Soc Pediatr Surg 9:605–620
Liem NT, le Dung A, Son TN (2009) Laparoscopic complete cyst excision and hepaticoduodenostomy for choledochal cyst: early results in 74 cases. J Laparoendosc Adv Surg Tech A 19(Suppl 1):S87-90
Todani T, Watanabe Y, Mizuguchi T et al (1981) Hepaticoduodenostomy at the hepatic hilum after excision of choledochal cyst. Am J Surg 142:584–587
Narayanan SK, Chen Y, Narasimhan KL et al (2013) Hepaticoduodenostomy versus hepaticojejunostomy after resection of choledochal cyst: a systematic review and meta-analysis. J Pediatr Surg 48:2336–2342
Farello GA, Cerofolini A, Rebonato M et al (1995) Congenital choledochal cyst: video-guided laparoscopic treatment. Surg Laparosc Endosc 5:354–358
Author information
Authors and Affiliations
Contributions
R.T., H.N., and T.D. wrote the main manuscript text and R.T., S.Y., T.O., and R.S. prepared figures and table. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tanaka, R., Nakamura, H., Yoshimoto, S. et al. Postoperative anastomotic stricture following excision of choledochal cyst: a systematic review and meta-analysis. Pediatr Surg Int 39, 30 (2023). https://doi.org/10.1007/s00383-022-05293-x
Accepted:
Published:
DOI: https://doi.org/10.1007/s00383-022-05293-x