Abstract
Purpose
The prenatal diagnosis of the stomach position in congenital diaphragmatic hernia (CDH) has been a reliable prognostic factor, but few studies have focused on the postnatal position. We therefore evaluated the significance of the nasogastric (NG) tube position just after birth.
Methods
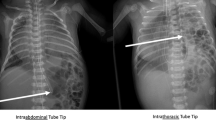
The Japanese CDH Study Group database enrolled 1037 CDH neonates over 15 years. In our multicenter retrospective study, 464 cases of left-sided isolated CDH with prenatal diagnoses were divided into two groups: NG tube below the diaphragm (BD; n = 190) or above the diaphragm (AD; n = 274). The primary outcome was the 90-day survival rate, and the secondary outcomes were mechanical ventilation duration, hospitalization duration, and recurrence rate.
Results
The BD group had a significantly higher 90-day survival rate (98.4 vs. 89.4%, p < 0.001), shorter mechanical ventilation (11 vs. 19 days, p < 0.001), shorter hospitalization (38 vs. 59 days, p < 0.001), and lower recurrence rate (p = 0.002) than the AD group. A multivariate analysis showed that BD (adjusted odds ratio, 3.68; 95% confidence interval 1.02–13.30) was a favorable prognostic factor for the 90-day survival.
Conclusion
The assessment of the NG tube position revealed it to be a reliable prognostic factor of left-sided isolated CDH. Therefore, it should be included as a routine assessment.


Similar content being viewed by others
Code availability
The datasets in this study are available from the corresponding author upon reasonable request.
Abbreviations
- CDH:
-
Congenital diaphragmatic hernia
- NG:
-
Nasogastric
- BD:
-
Below diaphragm
- AD:
-
Above diaphragm
- LHR:
-
Lung area-to-head circumference ratio
- o/eLHR:
-
Observed/expected lung area-to-head circumference ratio
- LTR:
-
Lung-to-thorax transverse ratio
- OI:
-
Oxygenation index
- iNO:
-
Inhaled nitric oxide
- ECMO:
-
Extracorporeal membrane oxygenation
- OR:
-
Odds ratio
- CI:
-
Confidence interval
References
Lansdale N, Alam S, Losty PD, Jesudason EC (2010) Neonatal endosurgical congenital diaphragmatic hernia repair: a systematic review and meta-analysis. Ann Surg 252:20–26. https://doi.org/10.1097/SLA.0b013e3181dca0e8
Dingeldein M (2018) Congenital diaphragmatic hernia: management and outcomes. Adv Pediatr 65:241–247
Congenital diaphragmatic hernia study group, Lally KP, Lally PA, Lasky RE et al (2007) Defect size determines survival in infants with congenital diaphragmatic hernia. Pediatrics 120:651–657. https://doi.org/10.1542/peds.2006-3040
Kirby E, Keijzer R (2020) Congenital diaphragmatic hernia: current management strategies from antenatal diagnosis to long-term follow-up. Pediatr Surg Int 36:415–429. https://doi.org/10.1007/s00383-020-04625-z
Keijzer R, Liu J, Deimling J et al (2000) Dual-hit hypothesis explains pulmonary hypoplasia in the nitrofen model of congenital diaphragmatic hernia. Am J Pathol 156:1299–1306. https://doi.org/10.1016/S0002-9440(10)65000-6
Cordier AG, Russo FM, Deprest J, Benachi A (2020) Prenatal diagnosis, imaging, and prognosis in congenital diaphragmatic hernia. Semin Perinatol 44:51163. https://doi.org/10.1053/j.semperi.2019.07.002
Dekoninck P, Gratacos E, Van Mieghem T et al (2011) Results of fetal endoscopic tracheal occlusion for congenital diaphragmatic hernia and the set up of the randomized controlled TOTAL trial. Early Hum Dev 87:619–624. https://doi.org/10.1016/j.earlhumdev.2011.08.001
Jani J, Nicolaides KH, Keller RL et al (2007) Observed to expected lung area to head circumference ratio in the prediction of survival in fetuses with isolated diaphragmatic hernia. Ultrasound Obstet Gynecol 30:67–71. https://doi.org/10.1002/uog.4052
Usui N, Kitano Y, Okuyama H et al (2011) Prenatal risk stratification for isolated congenital diaphragmatic hernia: results of a Japanese multicenter study. J Pediatr Surg 46:1873–1880. https://doi.org/10.1016/j.jpedsurg.2011.06.007
Kitano Y, Okuyama H, Saito M et al (2011) Re-evaluation of stomach position as a simple prognostic factor in fetal left congenital diaphragmatic hernia: a multicenter survey in Japan. Ultrasound Obstet Gynecol 37:277–282. https://doi.org/10.1002/uog.8892
Basta AM, Lusk LA, Keller RL, Filly RA (2016) Fetal stomach position predicts neonatal outcomes in isolated left-sided congenital diaphragmatic hernia. Fetal Diagn Ther 39:248–255. https://doi.org/10.1159/000440649
Terui K, Nagata K, Hayakawa M et al (2020) Novel risk score for fetuses with congenital diaphragmatic hernia based on ultrasound findings. Eur J Pediatr Surg 30:51–58. https://doi.org/10.1055/s-0039-1698768
Lally KP, Lasky RE, Lally PA et al (2013) Standardized reporting for congenital diaphragmatic hernia–an international consensus. J Pediatr Surg 48:2408–2415. https://doi.org/10.1016/j.jpedsurg.2013.08.014
Jancelewicz T, Brindle ME (2020) Prediction tools in congenital diaphragmatic hernia. Semin Perinatol 44:151165. https://doi.org/10.1053/j.semperi.2019.07.004
Hatch EI Jr, Kendall J, Blumhagen J (1992) Stomach position as an in utero predictor of neonatal outcome in left-sided diaphragmatic hernia. J Pediatr Surg 27:778–779. https://doi.org/10.1016/s0022-3468(05)80116-2
Mann PC, Morriss FH Jr, Klein JM (2012) Prediction of survival in infants with congenital diaphragmatic hernia based on stomach position, surgical timing, and oxygenation index. Am J Perinatol 29:383–390. https://doi.org/10.1055/s-0032-1304817
Kays DW, Islam S, Larson SD, Perkins J et al (2013) Long-term maturation of congenital diaphragmatic hernia treatment results: toward development of a severity-specific treatment algorithm. Ann Surg 258:638–644. https://doi.org/10.1097/SLA.0b013e3182a53c49
Grizelj R, Bojanić K, Vuković J, Novak M et al (2016) Epidemiology and outcomes of congenital diaphragmatic hernia in croatia: a population-based study. Paediatr Perinat Epidemiol 30:336–345. https://doi.org/10.1111/ppe.12289
Russo FM, Cordier AG, De Catte L et al (2018) Proposal for standardized prenatal ultrasound assessment of the fetus with congenital diaphragmatic hernia by the European reference network on rare inherited and congenital anomalies (ERNICA). Prenat Diagn 38:629–637. https://doi.org/10.1002/pd.5297
Global paedsurg research collaboration (2021) Mortality from gastrointestinal congenital anomalies at 264 hospitals in 74 low-income, middle-income, and high-income countries: a multicentre, international, prospective cohort study. Lancet 398:325–339. https://doi.org/10.1016/S0140-6736(21)00767-4
Acknowledgements
We thank Brian Quinn for English language editing. We also thank all members of the Japanese CDHSG for their commitments to CDH research.
Funding
This work was supported by a grant from the Ministry of Health, Labour and Welfare of Japan (Program Grant Number 20FC1017).
Author information
Authors and Affiliations
Contributions
KN: designed the study and JK: analyzed the data, and wrote the draft on the manuscript. KT, SA, KT, NI, YK, MY, TO, YY, HO, MH, TF, KM, AY, NU: contributed to the data collection, data cleaning, interpretation. KT, KT, HO, NU, and TT: critically reviewed this manuscript. The final version of the manuscript was approved by all authors.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to disclose.
Ethical approval
This study was approved by the ethics committee of Kyushu University (Ethical approval number 2020-759) and an institutional review board of all participating institutions.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kono, J., Nagata, K., Terui, K. et al. The efficacy of the postnatal nasogastric tube position as a prognostic marker of left-sided isolated congenital diaphragmatic hernia. Pediatr Surg Int 38, 1873–1880 (2022). https://doi.org/10.1007/s00383-022-05226-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-022-05226-8