Abstract
Purpose
We aimed to assess predictors of length of stay for simple gastroschisis utilizing the NSQIP-Pediatric Database.
Methods
The NSQIP-P Participant Use Data File was queried to identify patients with simple gastroschisis. We defined short length of stay (LOS) as patients discharged home ≤ 30 days from birth. We compared patients with short LOS versus prolonged LOS > 30 days. Predictors and outcomes were evaluated.
Results
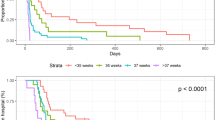
There were 888 patients with simple gastroschisis identified. Half of patients had LOS ≤ 30 days. Patients with LOS ≤ 30 were younger at repair (median age 1 day vs. 3 days, p = 0.0001), had higher birth weight (median 2.5 kg vs. 2.4 kg, p = 0.0001), and were less premature (37 week vs. 36 weeks, p = 0.0001). However, only gestational age and weight at birth were significant predictors of LOS on multivariate analysis (p = 0.0001). Prolonged LOS patients had more instances of ventilation, oxygen supplementation, sepsis (n = 2/446 or 0.4% vs. n = 9/442 or 2%, p = 0.003), bleeding/transfusion (n = 7/446 or 1.6% vs. n = 43/442 or 9.7%, p = 0.0001), line infections (n = 1/446 or 0.2% vs. n = 12/442, p = 0.001), and reoperations (n = 9/446 or 2% vs. n = 26/442 or 5.9%, p = 0.003).
Conclusion
Prematurity and birth weight are significant predictors of length of stay in simple gastroschisis patients. Prenatal counseling should continue to be one of the main factors to improve the outcomes for patients with gastroschisis.
Type of study Retrospective cohort study.
Level of evidence Level IV.

Similar content being viewed by others
References
Calderon MG, Santos EFS, Abreu LC, Raimundo RD (2019) Increasing prevalence, time trend and seasonality of gastroschisis in São Paulo state, Brazil, 2005–2016. Sci Rep 9(1):14491. https://doi.org/10.1038/s41598-019-50935-1
Mastroiacovo P (2008) Risk factors for gastroschisis. BMJ 336(7658):1386–1387. https://doi.org/10.1136/bmj.39577.589699.BE
Kunz SN, Tieder JS, Whitlock K et al (2013) Primary fascial closure versus staged closure with silo in patients with gastroschisis: a meta-analysis. J Pediatr Surg 48(4):845–857. https://doi.org/10.1016/j.jpedsurg.2013.01.020
Badrinath R, Kakembo N, Kisa P et al (2014) Outcomes and unmet need for neonatal surgery in a resource-limited environment: estimates of global health disparities from Kampala, Uganda. J Pediatr Surg 49(12):1825–1830. https://doi.org/10.1016/j.jpedsurg.2014.09.031
Snyder CW, Biggio JR, Brinson P, Barnes LA, Bartle DT, Georgeson KE, Muensterer OJ (2011) Effects of multidisciplinary prenatal care and delivery mode on gastroschisis outcomes. J Pediatr Surg 46(1):86–89. https://doi.org/10.1016/j.jpedsurg.2010.09.067. Erratum in: J Pediatr Surg. 2011;46(8):1685. Synder, Christopher W [corrected to Snyder, Christopher W]
Youssef F, Cheong LH, Emil S, Canadian Pediatric Surgery Network (CAPSNet) (2016) Gastroschisis outcomes in North America: a comparison of Canada and the United States. J Pediatr Surg 51(6):891–895. https://doi.org/10.1016/j.jpedsurg.2016.02.046
Bruzoni M, Jaramillo JD, Dunlap JL et al (2017) Sutureless vs sutured gastroschisis closure: a prospective randomized controlled trial. J Am Coll Surg 224(6):1091-1096.e1. https://doi.org/10.1016/j.jamcollsurg.2017.02.014
Overcash RT, Degarte DA, Stephenson ML et al (2014) University of California Fetal Consortium*. Factors associated with gastroschisis outcomes. Obstet Gynecol 124(3):551–557. https://doi.org/10.1097/AOG.0000000000000425
Puligandla PS, Janvier A, Flageole H et al (2004) The significance of intrauterine growth restriction is different from prematurity for the outcome of infants with gastroschisis. J Pediatr Surg 39(8):1200–1204. https://doi.org/10.1016/j.jpedsurg.2004.04.014
Fraga MV, Laje P, Peranteau WH, Hedrick HL, Khalek N, Gebb JS, Moldenhauer JS, Johnson MP, Flake AW, Adzick NS (2018) The influence of gestational age, mode of delivery and abdominal wall closure method on the surgical outcome of neonates with uncomplicated gastroschisis. Pediatr Surg Int 34(4):415–419. https://doi.org/10.1007/s00383-018-4233-5
Ergün O, Barksdale E, Ergün FS et al (2005) The timing of delivery of infants with gastroschisis influences outcome. J Pediatr Surg 40(2):424–428. https://doi.org/10.1016/j.jpedsurg.2004.10.013
Salihu HM, Emusu D, Aliyu ZY et al (2004) Mode of delivery and neonatal survival of infants with isolated gastroschisis. Obstet Gynecol 104(4):678–683. https://doi.org/10.1097/01.AOG.0000139513.93115.81
Charlesworth P, Njere I, Allotey J et al (2007) Postnatal outcome in gastroschisis: effect of birth weight and gestational age. J Pediatr Surg 42(5):815–818. https://doi.org/10.1016/j.jpedsurg.2006.12.034
Freitas AB, Centofanti SF, Osmundo-Junior GS et al (2020) Risk factors for gastroschisis: a case-control study in a Brazilian population. Int J Gynaecol Obstet 149(3):347–353. https://doi.org/10.1002/ijgo.13135
Baldacci S, Santoro M, Coi A et al (2020) Lifestyle and sociodemographic risk factors for gastroschisis: a systematic review and meta-analysis. Arch Dis Child 105(8):756–764. https://doi.org/10.1136/archdischild-2019-318412
David AL, Tan A, Curry J (2008) Gastroschisis: sonographic diagnosis, associations, management and outcome. Prenat Diagn 28(7):633–644. https://doi.org/10.1002/pd.1999
Rittler M, Campaña H, Heisecke S et al (2021) Lethality of birth defects in live born infants categorized by gestational age and birth weight. Am J Perinatol. https://doi.org/10.1055/s-0041-1735867
Carnaghan H, Pereira S, James CP et al (2014) Is early delivery beneficial in gastroschisis? J Pediatr Surg 49(6):928–933. https://doi.org/10.1016/j.jpedsurg.2014.01.027
Passaro RC, Savoie KB, Huang EY (2018) Use of a gastroschisis feeding guideline to improve standardization of care and patient outcomes at an urban Children’s hospital. Nutr Clin Pract 33(4):545–552. https://doi.org/10.1002/ncp.10083
Walter-Nicolet E, Rousseau V, Kieffer F et al (2009) Neonatal outcome of gastroschisis is mainly influenced by nutritional management. J Pediatr Gastroenterol Nutr 48(5):612–617. https://doi.org/10.1097/MPG.0b013e31818c5281
Lemoine JB, Smith RR, White D (2015) Got milk? Effects of early enteral feedings in patients with gastroschisis. Adv Neonatal Care 15(3):166–175. https://doi.org/10.1097/ANC.0000000000000171
Financial support
No financial support was granted this study. All authors have no financial support to disclose.
Author information
Authors and Affiliations
Contributions
Conceptualization: Gustavo Villalona; Methodology: Gustavo Villalona, Adam Bajinting; Data Acquisition: Pattamon Sutthatarn, Hector Osei, Armando Salim Munoz Abraham, Adam Bajinting; Formal analysis and investigation: Adam Bajinting; Writing—original draft preparation: Adam Bajinting; Writing—review and editing: Adam Bajinting, Gustavo Villalona; Supervision: Gustavo Villalona.
Corresponding author
Ethics declarations
Competing interests
All authors declare no competing interests.
Compliance and ethical standards
Saint Louis University IRB does not require IRB approval or exemption to use the ACS NSQIP-P Database, since it is a secondary-deidentified-publicly available data, and it does not meet their definition of Human Subjects Research.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bajinting, A., Sutthatarn, P., Osei, H. et al. Predictors of length of stay for simple gastroschisis: analysis of ACS NSQIP-P database. Pediatr Surg Int 38, 1371–1376 (2022). https://doi.org/10.1007/s00383-022-05189-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-022-05189-w