Abstract
Introduction
This study tested the hypothesis that complication accrual during pediatric extracorporeal life support (ECLS) increases mortality irrespective of indication for support.
Methods
Prospectively collected Extracorporeal Life Support Organization (ELSO) registry data for all neonatal and pediatric patients cannulated for ECLS at our institution from 1/1/2015 to 12/31/2020 was stratified based on the presence or absence of complications. We excluded renal replacement therapy from complications, as this is frequently and empirically applied within our practice.
Results
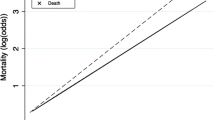
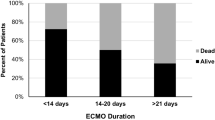
Of 114 patients, overall survival to discharge was 66%. 62 patients (54%) had 149 total complications: 29% were mechanical (circuit related), and the rest were patient related. Age (neonatal versus pediatric), sex, race/ethnicity, support type, presence of pre-ECLS arrest, pre-ECLS pH and intubation-to-ECLS duration were not significantly associated with the development of complications. Patients with complications required longer ECLS duration (168 versus 86 median hours, p < 0.001) and were more likely to be decannulated due to death or poor prognosis (25% versus 8%, p = 0.022). One or more ECLS complications was associated with significantly decreased survival by Cox proportional hazard regression (p = 0.003).
Conclusion
Complications on ECLS are associated with longer support duration and predict decreased survival independent of pre-ECLS variables, suggesting a multidisciplinary ECLS team target for improved outcomes.


Similar content being viewed by others
Notes
Renal replacement therapy is defined in the ELSO registry database as Peritoneal Dialysis, Continuous Venovenous Hemodiafiltration (CVVHD), Continuous Venovenous Hemofiltration (CVVHF) or Continuous Venovenous Hemodiafiltration (CVVHDF) or Hemodialysis (HD) based on the patient's ultimate mode of therapy. At our institution, we empirically utilize CVVHD.
References
Maul TM, Aspenleiter M, Palmer D, Sharma MS, Viegas ML, Wearden PD (2020) Impact of circuit size on coagulation and hemolysis complications in pediatric extracorporeal membrane oxygenation. Asaio J 66(9):1048–1053
Nasr VG, Faraoni D, DiNardo JA, Thiagarajan RR (2016) Association of hospital structure and complications with mortality after pediatric extracorporeal membrane oxygenation. Pediatr Crit Care Med 17(7):684–691
Niebler RA, Parker H, Hoffman GM (2019) Impact of anticoagulation and circuit technology on complications during extracorporeal membrane oxygenation. Asaio J 65(3):270–276
Rama G, Middlesworth W, Neunert C, Streltsova S, Cheung EW (2021) Antifactor Xa monitoring and hematologic complications of pediatric extracorporeal membrane oxygenation. Asaio J 67(1):91–95
Said AS, Guilliams KP, Bembea MM (2020) Neurological monitoring and complications of pediatric extracorporeal membrane oxygenation support. Pediatr Neurol 108:31–39
Thomas J, Kostousov V, Teruya J (2018) Bleeding and thrombotic complications in the use of extracorporeal membrane oxygenation. Semin Thromb Hemost 44(1):20–29
Fallon BP, Gadepalli SK, Hirschl RB (2021) Pediatric and neonatal extracorporeal life support: current state and continuing evolution. Pediatr Surg Int 37(1):17–35
Glenn IC, Abdulhai S, Lally PA, Schlager A (2019) Early CDH repair on ECMO: improved survival but no decrease in ECMO duration (A CDH Study Group Investigation). J Pediatr Surg 54(10):2038–2043
Trivedi P, Glass K, Clark JB, Myers JL, Cilley RE, Ceneviva G, Wang S, Kunselman AR, Ündar A (2019) Clinical outcomes of neonatal and pediatric extracorporeal life support: a seventeen-year, single institution experience. Artif Organs 43(11):1085–1091
Lin JC (2017) Extracorporeal membrane oxygenation for severe pediatric respiratory failure. Respir Care 62(6):732–750
Maslach-Hubbard A, Bratton SL (2013) Extracorporeal membrane oxygenation for pediatric respiratory failure: history, development and current status. World J Crit Care Med 2(4):29–39
Gupta P, McDonald R, Chipman CW, Stroud M, Gossett JM, Imamura M, Bhutta AT (2012) 20-year experience of prolonged extracorporeal membrane oxygenation in critically ill children with cardiac or pulmonary failure. Ann Thorac Surg 93(5):1584–1590
Acknowledgements
There was no source of funding for this research.
Author information
Authors and Affiliations
Contributions
Study conception and design: LEH; data acquisition: LEA and LEH; analysis and data interpretation: LEA, LEH, and RM; drafting of the manuscript: LEA, LEH, and RM; critical revision: LEA, LEH, and RM.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors declare no financial conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Adams, L.E., Mukherjee, R. & Hollinger, L.E. Complication accrual impacts pediatric extracorporeal life support mortality. Pediatr Surg Int 38, 985–991 (2022). https://doi.org/10.1007/s00383-022-05140-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-022-05140-z