Abstract
Purpose
To investigate the occupational and environmental factors in the etiology of infantile hypertrophic pyloric stenosis (IHPS).
Methods
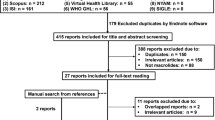
Protocol was drafted according to the PRISMA guidelines and registered on PROSPERO (CRD42020152460). A search for a combination of terms related to IHPS, fetus and neonates, and environmental exposure was performed for studies published between 2000 and 2020 in the EMBASE, Pubmed, and MEDLINE databases.
Results
Overall, 2203 abstracts were identified and 829 were screened. The full text of the selected articles (N = 98) was assessed for eligibility. Fifteen studies were included in quantitative synthesis. IHPS risk was significantly lower in black and Hispanic mothers than in white mothers [OR 0.47 (95% CI 0.44–0.51, p < 0.001), OR 0.85 (95% CI 0.77–0.94, p = 0.002), respectively]. Lower maternal education level and maternal smoking were risk factor for IHPS. We further observed a non-significant association between maternal folic acid usage and IHPS risk. Data were insufficient to evaluate occupational exposure.
Conclusion
This review provides an understanding of the role of environmental exposures in IHPS etiology. Lower maternal educational level, maternal smoking, and white ethnicity are associated with a significantly increased risk of IHPS, while folic acid use seems non-significantly associated with IHPS risk.
Level of evidence
III.




Similar content being viewed by others
References
El-Gohary Y, Abdelhafeez A, Paton E et al (2018) Pyloric stenosis: an enigma more than a century after the first successful treatment. Pediatr Surg Int 34:21–27
Georgoula C, Gardiner M (2012) Pyloric stenosis a 100 years after Ramstedt. Arch Dis Child 97:741–745
Ranells JD, Carver JD, Kirby RS (2011) Infantile hypertrophic pyloric stenosis: Epidemiology, genetics, and clinical update. Adv Pediatr 58:195–206
MacMahon B (2006) The continuing enigma of pyloric stenosis of infancy: a review. Epidemiology 17:195–201
Zhu J, Zhu T, Lin ZL et al (2017) Perinatal risk factors for infantile hypertrophic pyloric stenosis: a meta-analysis. J Pediatr Surg 52:1389–1397
Abdellatif M, Ghozy S, Kamel MG et al (2018) Association between exposure to macrolides and the development of infantile hypertrophic pyloric stenosis: a systematic review and meta-analysis. Eur J Pediatr. https://doi.org/10.1007/s00431-018-3287-7
Murchison L, De Coppi P, Eaton S (2016) Post-natal erythromycin exposure and risk of infantile hypertrophic pyloric stenosis: a systematic review and meta-analysis. Pediatr Surg Int 32:1147–1152
Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71. https://doi.org/10.1136/bmj.n71
Boybeyi-Turer O, Celik HT, Arslan UE et al (2021) Protocol: a systematic review and meta-analysis of the role of fetal and infantile environmental exposure in etiopathogenesis of infantile hypertrophic pyloric stenosis. PLoS ONE. https://doi.org/10.1371/journal.pone.0247003
Ijaz S, Verbeek J, Seidler A et al (2013) Night-shift work and breast cancer—a systematic review and meta-analysis. Scand J Work Environ Health 39:431–447
Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50:1088–1101
Duval S, Tweedie R (2000) Trim and fill: a simple funnel-plot based method of testing and adjusting for publication bias in meta- analysis. Biometrics 56:455–463
Egger M, Davey Smith G, Schneider M et al (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315:629–634
Wang J, Waller DK, Hwang LY et al (2008) Prevalence of infantile hypertrophic pyloric stenosis in Texas, 1999–2002. Birth Defects Res (Part A) 82:763–767
Canfield MA, Collins JS, Botto LD et al (2005) Changes in the birth prevalence of selected birth defects after grain fortification with folic acid in the United States: findings from a multi-state population-based study. Birth Defects Res (Part A) 73:679–689
Kapoor R, Kancherla V, Cao Y et al (2019) Prevalence and descriptive epidemiology of infantile hypertrophic pyloric stenosis in the United States: a multistate, population-based retrospective study, 1999–2010. Birth Defects Res 111:159–169
Lin KJ, Mitchell AA, Yau WP et al (2013) Safety of macrolides during pregnancy. Am J Obstet Gynecol 208:221.e1-e8
Lisonkova S, Joseph KS (2014) Similarities and differences in the epidemiology of pyloric stenosis and SIDS. Matern Child Health J 18:1721–1727
McAteer JP, Ledbetter DJ, Goldin AB (2013) Role of bottle feeding in the etiology of hypertrophic pyloric stenosis. JAMA Pediatr 167:1143–1149
Markel TA, Proctor C, Ying J et al (2015) Environmental pesticides increase the risk of developing hypertrophic pyloric stenosis. J Pediatr Surg 50:1283–1288
Kirby RS, Mai CT, Wingate MS et al (2019) Prevalence of selected birth defects by maternal nativity status, United States, 1999–2007. Birth Defects Res 111:630–639
Svenningsson A, Svensson T, Akre O et al (2014) Maternal and pregnancy characteristics and risk of infantile hypertrophic pyloric stenosis. J Pediatr Surg 49:1226–1231
Sorensen HT, Norgard B, Pedersen L et al (2002) Maternal smoking and risk of hypertrophic infantile pyloric stenosis: 10 year population based cohort study. BMJ 325:1011–1012
Bakker MK, De Walle HEK, Wilffert B et al (2010) Fluoxetine and infantile hypertrophic pylorus stenosis: a signal from a birth defects-drug exposure surveillance study. Pharmacoepidemiol Drug Saf 19:808–813
Krogh C, Gortz S, Wohlfahrt J et al (2012) Pre- and perinatal risk factors for pyloric stenosis and their influence on the male predominance. Am J Epidemiol 176:24–31
Leite M, Albieri V, Kjaer SK et al (2014) Maternal smoking in pregnancy and risk for congenital malformations: results of a Danish register-based cohort study. Acta Obstet Gynecol Scand 93:825–834
Vermes G, László D, Czeizel AE et al (2016) Maternal factors in the origin of infantile hypertrophic pyloric stenosis: a population-based case–control study. Congenit Anom 56:65–72
Rosenthal YS, Chodick G, Grossman Z et al (2019) The incidence of infantile hypertrophic pyloric stenosis and its association with folic acid supplementation during pregnancy: a nested case–control study. J Pediatr Surg 54:701–706
Li J, Gao W, Zhu J et al (2018) Epidemiological and clinical characteristics of 304 patients with infantile hypertrophic pyloric stenosis in Anhui Province of East China, 2012–2015. J Maternal-Fetal Neonatal Med 31:2742–2747
Sommerfield T, Chalmers J, Youngson G et al (2008) The changing epidemiology of infantile hypertrophic pyloric stenosis in Scotland. Arch Dis Child 93:1007–1011
Nielsen JP, Haahr P, Haahr J (2000) Infantile hypertrophic pyloric stenosis. Decreasing incidence. Dan Med Bull 47:223–225
Persson S, Ekbom A, Granath F et al (2001) Parallel incidences of sudden infant death syndrome and infantile hypertrophic pyloric stenosis: a common cause? Pediatrics 108:e70
Pedersen RN, Garne E, Loane M et al (2008) Infantile hypertrophic pyloric stenosis: a comparative study of incidence and other epidemiological characteristics in seven European regions. J Matern Fetal Neonatal Med 21:599–604
Acs N, Banhidy F, Puho EH et al (2009) Senna treatment in pregnant women and congenital abnormalities in their offspring—a population-based case–control study. Reprod Toxicol 28:100–104
Yau W, Mitchell AA, Lin KJ et al (2013) Use of decongestants during pregnancy and the risk of birth defects. Am J Epidemiol 178:198–208
Block SR, Watkins SM, Salemi JL et al (2013) Maternal pre-pregnancy body mass index and risk of selected birth defects: evidence of a dose-response relationship. Paediatr Perinat Epidemiol 27:521–531
Grewal J, Carmichael SL, Yang W et al (2012) Paternal age and congenital malformations in offspring in California, 1989–2002. Matern Child Health J 16:385–392
Olshan AF, Teschke K, Baird PA (1991) Paternal occupation and congenital anomalies in offspring. Am J Ind Med 20:447–475
Acknowledgements
The study protocol was registered on PROSPERO (Registration Number: CRD42020152460). The manuscript was edited by Hacettepe Technopolis Technology Transfer Center (HT-TTM).
Funding
The study is supported by Hacettepe University, Scientific Research Council (Grant Number: 18121).
Author information
Authors and Affiliations
Contributions
The authors contributed to the study as following: (i) conception and design: all authors, (ii) materials, investigations and literature search: B-TO, CHT, ST, and AUE, (iii) analysis and interpretation: AUE, B-TO, and ST, (iv) writer and supervision: B-TO, KS, and CHT, and (v) critical review: ST, TFC, and KS.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that there is no conflict of interest.
Ethical considerations
Formal ethical approval is not required for this study. An institutional collaboration is approved by the Local Ethical Committee (11/12/2018-2230) revealing that this study does not need an ethical approval.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Feridun Cahit Tanyel: Member of Turkey Academy of Sciences, Ankara, Turkey.
Rights and permissions
About this article
Cite this article
Boybeyi-Turer, O., Celik, H.T., Arslan, U.E. et al. Environmental exposure in the etiology of infantile hypertrophic pyloric stenosis: a systematic review and meta-analysis. Pediatr Surg Int 38, 951–961 (2022). https://doi.org/10.1007/s00383-022-05128-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-022-05128-9