Abstract
Introduction
Pediatric bowel obstruction after intra-abdominal cancer surgery is relatively frequent. Few publications have specifically addressed this significant complication. The purpose of this study was to assess the frequency, etiology and treatment options of bowel obstructions following abdominal cancer surgery in children using our institutional database.
Materials and Methods
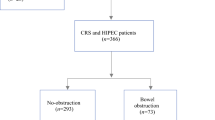
We retrospectively analyzed a single tertiary pediatric hospital database over a 10-year period. The clinical characteristics of patients with and without bowel obstruction were compared using bivariate analyses. The details of the conservative and operative management of bowel obstructions were evaluated.
Results
Out of 130 eligible patients, 18 (13.8%) developed bowel obstruction in a mean follow-up of 5.7 years. Patients who developed bowel obstruction were more likely to have received preoperative radiation therapy (16.7 vs 2.7%, p = 0.036) and had longer operative time (398 vs 268 min, p = 0.022). Non-operative management was successful in 39% of patients (7/18). When patients needed surgical intervention, minimally invasive approach was attempted and successfully performed in 36% of cases (4/11), none of which required conversion to laparotomy nor presented with recurrent bowel obstruction.
Conclusion
Bowel obstruction is a frequent complication after abdominal cancer surgery in children. Conservative management is frequently successful. For patients requiring surgical treatment, laparoscopy remains a valuable option and should be considered in selected cases.
Similar content being viewed by others
References
Lakshminarayanan B, Hughes-Thomas AO, Grant HW (2014) Epidemiology of adhesions in infants and children following open surgery. Semin Pediatr Surg 23(6):344–348. https://doi.org/10.1053/j.sempedsurg.2014.06.005
Lautz TB, Barsness KA (2014) Adhesive small bowel obstruction–acute management and treatment in children. Semin Pediatr Surg 23(6):349–352. https://doi.org/10.1053/j.sempedsurg.2014.06.006
Aguayo P, Ho B, Fraser JD, Gamis A, St Peter SD, Snyder CL (2010) Bowel obstruction after treatment of intra-abdominal tumors. Eur J Pediatr Surg 20(4):234–236. https://doi.org/10.1055/s-0030-1253401
Madenci AL, Fisher S, Diller LR, Goldsby RE, Leisenring WM, Oeffinger KC, Robison LL, Sklar CA, Stovall M, Weathers RE, Armstrong GT, Yasui Y, Weldon CB (2015) Intestinal obstruction in survivors of childhood cancer: a report from the childhood cancer survivor study. J Clin Oncol 33(26):2893–2900. https://doi.org/10.1200/JCO.2015.61.5070
Ritchey ML, Kelalis PP, Etzioni R, Breslow N, Shochat S, Haase GM (1993) Small bowel obstruction after nephrectomy for Wilms’ tumor. A report of the National Wilms’ Tumor Study-3. Ann Surg 218(5):654–659
Bower KL, Lollar DI, Williams SL, Adkins FC, Luyimbazi DT, Bower CE (2018) Small Bowel Obstruction. Surg Clin North Am 98(5):945–971. https://doi.org/10.1016/j.suc.2018.05.007
Andreyev HJ (2007) Gastrointestinal problems after pelvic radiotherapy: the past, the present and the future. Clin Oncol (R Coll Radiol) 19(10):790–799. https://doi.org/10.1016/j.clon.2007.08.011
Theis VS, Sripadam R, Ramani V, Lal S (2010) Chronic radiation enteritis. Clin Oncol (R Coll Radiol) 22(1):70–83. https://doi.org/10.1016/j.clon.2009.10.003
Husaric E, Hasukic S, Hotic N, Halilbasic A, Husaric S, Hasukic I (2016) Risk factors for post-colectomy adhesive small bowel obstruction. Acta Med Acad 45(2):121–127. https://doi.org/10.5644/ama2006-124.167
Hyak J, Campagna G, Johnson B, Stone Z, Yu Y, Rosenfeld E, Zhang W, Naik-Mathuria B (2019) Management of pediatric adhesive small bowel obstruction: do timing of surgery and age matter? J Surg Res 243:384–390. https://doi.org/10.1016/j.jss.2019.05.061
Sajid MS, Khawaja AH, Sains P, Singh KK, Baig MK (2016) A systematic review comparing laparoscopic vs open adhesiolysis in patients with adhesional small bowel obstruction. Am J Surg 212(1):138–150. https://doi.org/10.1016/j.amjsurg.2016.01.030
Sebastian-Valverde E, Poves I, Membrilla-Fernandez E, Pons-Fragero MJ, Grande L (2019) The role of the laparoscopic approach in the surgical management of acute adhesive small bowel obstruction. BMC Surg 19(1):40. https://doi.org/10.1186/s12893-019-0504-x
Miyake H, Seo S, Pierro A (2018) Laparoscopy or laparotomy for adhesive bowel obstruction in children: a systematic review and meta-analysis. Pediatr Surg Int 34(2):177–182. https://doi.org/10.1007/s00383-017-4186-0
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Habti, M., Miyata, S., Côté, J. et al. Bowel obstruction following pediatric abdominal cancer surgery. Pediatr Surg Int 38, 1041–1045 (2022). https://doi.org/10.1007/s00383-022-05127-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-022-05127-w