Abstract
Purpose
The present study aimed to explore the clinical characteristics and optimal treatments of RHB patients.
Methods
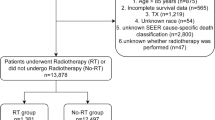
We retrospectively collected 42 RHB cases and 161 primary HB (PHB) cases. Clinical characteristics were compared between RHB and PHB patients. The risk factors related to overall survival (OS) and progression-free survival (PFS) in RHB patients were explored by COX regression analysis. Patients were further divided into curable and refractory subgroup by treatments. Propensity score match (PSM) analysis was performed to match recurrent curable patients from 145 curable PHB patients from the same cohort. PFS was further compared between 34 pairs of primary and recurrent curative HB patients.
Results
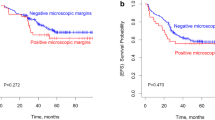
Recurrence treatment and number of relapsed tumors were significantly related with both OS and PFS of RHB patients (p < 0.05). Chemotherapy regimen alteration was also risk factor of PFS for RHB (HR = 4.26; 95% CI = 1.54–11.78; p = 0.005). RHB patients underwent curable treatment had better prognosis, compared with recurrent refractory subgroup (p < 0.001). Matched curable PHB patients demonstrated no significant difference of 3-year PFS with curable RHB patients (p = 0.540).
Conclusion
Curable RHB patients might get benefit from surgery or ablation with similar prognosis with primary curable HB patients.


Similar content being viewed by others
References
Hooks A, Fazli L, Ernault D-S et al (2018) New insights into diagnosis and therapeutic options for proliferative hepatoblastoma. Hepatology 68:89–102. https://doi.org/10.1002/hep.29672
Siegel RL, Miller KD, Jemal A (2019) Cancer statistics, 2019. CA Cancer J Clin 69:7–34. https://doi.org/10.3322/caac.21551
Shi C, Masand H, Goss V (2017) Vascular invasion is a prognostic indicator in hepatoblastoma. J Pediatr Surg 52:956–961. https://doi.org/10.1016/j.jpedsurg.2017.03.017
Trobaugh-Lotrario AD, Meyers RL, Feusner JH (2016) Outcomes of patients with relapsed hepatoblastoma enrolled on Children’s Oncology Group (COG) phase i and ii studies. J Pediatr Hematol Oncol 38:187–190. https://doi.org/10.1097/mph.0000000000000474
Zhang C, Yao Li, Zhong L (2020) Novel treatment of refractory/recurrent pulmonary hepatoblastoma. Pediatr Int 62:324–329. https://doi.org/10.1111/ped.14134
Venkatramani R, Furman WL, Fuchs J, Warmann SW, Malogolowkin MH (2012) Current and future management strategies for relapsed or progressive hepatoblastoma. Paediatr Drugs 14:221–232. https://doi.org/10.2165/11597740-000000000-00000
Hou JY, Yeh TC, Huang TH, Sheu JC, Liu HC (2021) A retrospective study of clinical features and outcome in patients with refractory or recurrent hepatoblastoma: a single institution experience. Pediatr Neonatol 62:400–405. https://doi.org/10.1016/j.pedneo.2021.03.018
Agarwala G, Bansal V, Prasad A et al (2017) Management of hepatoblastoma: ICMR consensus document. Indian J Pediatr 84:456–464. https://doi.org/10.1007/s12098-017-2301-9
Semeraro B, Maibach Z, Casanova B et al (2013) Relapses in hepatoblastoma patients: clinical characteristics and outcome–experience of the International Childhood Liver Tumour Strategy Group (SIOPEL). Eur J Cancer 49:915–922. https://doi.org/10.1016/j.ejca.2012.10.003
Hetzer V, Entenmann H, Schullian P et al (2020) Stereotactic radiofrequency ablation of a variety of liver masses in children. Int J Hyperth 37:1074–1081. https://doi.org/10.1080/02656736.2020.1822549
Yevich C, Gravel F, Brugières V-C et al (2019) Reiterative radiofrequency ablation in the management of pediatric patients with hepatoblastoma metastases to the lung, liver, or bone. Cardiovasc Intervent Radiol 42:41–47. https://doi.org/10.1007/s00270-018-2097-7
Cui Yu, Gu C, Liu D et al (2019) Microwave ablation assisted by three-dimensional visualization system as local therapy for relapsed hepatoblastoma: a small pilot study. Abdominal Radiol 44:2909–2915. https://doi.org/10.1007/s00261-019-02011-5
Chinese Anti-Cancer Association Pediatric Committee, China Medical Association Pediatric Onco-surgery Group (2017) Expert consensus for multidisciplinary management of hepatoblastoma (CCCG-HB-2016). Chin J Pediatr Surg 38:733–739
Eisenhauer T, Bogaerts S, Sargent F et al (2009) New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 45:228–247. https://doi.org/10.1016/j.ejca.2008.10.026
Meyers M, Hiyama H, Krailo R et al (2017) Risk-stratified staging in paediatric hepatoblastoma: a unified analysis from the Children’s Hepatic tumors International Collaboration. Lancet Oncol 18:122–131. https://doi.org/10.1016/s1470-2045(16)30598-8
Chen H, Ling Yu, Cheng L et al (2021) Percutaneous thermal ablation versus open liver resection for recurrent hepatoblastoma: a retrospective study. Int J Hyperth 38:1086–1091. https://doi.org/10.1080/02656736.2021.1941310
Liu Z, Huang Z, Jiang S et al (2015) First experience of ultrasound-guided percutaneous ablation for recurrent hepatoblastoma after liver resection in children. Sci Rep 5:16805. https://doi.org/10.1038/srep16805
Hirsch P, Morcrette R, Monteiro M et al (2021) Integrated genomic analysis identifies driver genes and cisplatin-resistant progenitor phenotype in pediatric liver cancer. Cancer Discov 11:2524–2543. https://doi.org/10.1158/2159-8290.CD-20-1809
Sumazin C, Treviño S, Hampton P et al (2017) Genomic analysis of hepatoblastoma identifies distinct molecular and prognostic subgroups. Hepatology 65:104–121. https://doi.org/10.1002/hep.28888
Gay S, Park D, Groves H et al (2021) Patterns of transcription factor programs and immune pathway activation define four major subtypes of SCLC with distinct therapeutic vulnerabilities. Cancer Cell 39(346–360):e347. https://doi.org/10.1016/j.ccell.2020.12.014
Czauderna H, Hiyama R, Krailo M et al (2016) The Children’s Hepatic tumors International Collaboration (CHIC): Novel global rare tumor database yields new prognostic factors in hepatoblastoma and becomes a research model. Eur J Cancer 52:92–101. https://doi.org/10.1016/j.ejca.2015.09.023
Sato K, Suzushino K, Okada I et al (2021) Predicting post-hepatectomy liver failure using intra-operative measurement of indocyanine green clearance in anatomical hepatectomy. World J Surg 45:3660–3667. https://doi.org/10.1007/s00268-021-06289-9
Chen Wu, Cheng W, Rong Wu et al (2021) Phase 2 study of adjuvant radiotherapy following narrow-margin hepatectomy in patients with HCC. Hepatology 74:2595–2604. https://doi.org/10.1002/hep.31993
Xia Li, Liu W, Qian Lu et al (2020) Long-term effects of repeat hepatectomy vs percutaneous radiofrequency ablation among patients with recurrent hepatocellular carcinoma: a randomized clinical trial. JAMA Oncol 6:255–263. https://doi.org/10.1001/jamaoncol.2019.4477
Funding
This work was supported by China Postdoctoral Science Foundation (2021M693650).
Author information
Authors and Affiliations
Contributions
YW, HJ, LH and HC designed the whole research. YL, LH, ZZ, PG, ZZ, JS and JL collected data. YL, YW and HC performed data interpretation and analysis. YW, HX, XW, HC and YL wrote the main manuscript text. HJ and LH gave critical revision. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors have no competing interests to declare that are relevant to the content of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wang, Y., Chen, H., Liu, Y. et al. Treatment optimization for recurrent hepatoblastoma: retrospective study from a hepatoblastoma cohort in Southern China. Pediatr Surg Int 38, 1031–1039 (2022). https://doi.org/10.1007/s00383-022-05126-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-022-05126-x