Abstract
Introduction
Neurogenic bladder with anorectal malformations (ARM) is a well-known yet understudied topic. Diffusion tensor imaging (DTI) is a special usage of MRI that can evaluate peripheric nerves. The aim of this study is to evaluate the lumbosacral plexuses of patients with ARM using DTI.
Patients and methods
Patients with ARM willing to participate were included. Patient files were reviewed, a questionnaire was made, and DTI was performed. Fractional anisotropy (FA) and apparent diffusion coefficient (ADC) were computed for the right and left lumbosacral plexuses.
Results
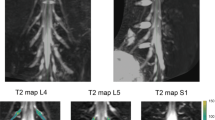
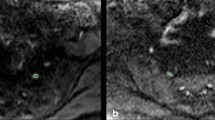
There were 18 patients and 12 controls. Groups were similar in terms of sex (p = 0.232) and age (p = 0.853). There was a significant difference only for ADC of the left plexus. There was visible asymmetry in tractographies and DTI parameters of two patients with severely deformed pelvises (image 1) but also in another patient with a normal sacrum. In addition, despite asymmetry, FA and ADC were similar to controls also in these patients.
Conclusion
This is the first study presenting quantitative data about the lumbosacral plexus in ARM. We think the most interesting finding of this study was observing the normal values even in the patients with severely malformed sacrum which is yet to be validated with further studies.

Similar content being viewed by others
References
Peña A, Bischoff A (2015) Urologic problems in anorectal malformations. Surgical treatment of colorectal problems in children. Springer, Cham, pp 371–396
Goossens WJH, De Blaauw I, Wijnen MH, De Gier RPE, Kortmann B, Feitz WFJ (2011) Urological anomalies in anorectal malformations in the Netherlands: effects of screening all patients on long-term outcome. Pediatr Surg Int 27:1091–1097. https://doi.org/10.1007/s00383-011-2959-4
Mosiello G, Capitanucci ML, Gatti C, Adorisio O, Lucchetti MC, Silveri M et al (2003) How to investigate neurovesical dysfunction in children with anorectal malformations. J Urol 170:1610–1613. https://doi.org/10.1097/01.ju.0000083883.16836.91
Pena A (1995) Anorectal malformations. J Jpn Soc Pediatr Surg 31:718–731
Haakma W, Dik P, Ten Haken B, Froeling M, Nievelstein RAJ, Cuppen I et al (2014) Diffusion tensor magnetic resonance imaging and fiber tractography of the sacral plexus in children with spina bifida. J Urol 192:927–933. https://doi.org/10.1016/j.juro.2014.02.2581
Tiryaki S, Eraslan C, Soyer T, Calli C, Ulman I, Avanoglu A (2019) Nonneuropathic neuropathic bladder: is it really nonneuropathic? J Urol 201:802–809. https://doi.org/10.1016/j.juro.2018.09.046
Rentea RM, Halleran DR, Vilanova-Sánchez A (2020) Antegrade access as an adjunct to bowel management: appendicostomy and neoappendicostomy. In: Vilanova-Sánchez A, Levitt MA (eds) Pediatric colorectal and pelvic reconstructive surgery, 1st edn. Taylor & Francis, Boca Raton, pp 137–146
Ochi T, Okazaki T, Miyano G, Lane GJ, Yamataka A (2012) A comparison of clinical protocols for assessing postoperative fecal continence in anorectal malformation. Pediatr Surg Int 28:1–4. https://doi.org/10.1007/s00383-011-2997-y
Brandt ML, Daigneau C, Graviss EA, Naik-Mathuria B, Fitch ME, Washburn KK (2007) Validation of the Baylor Continence Scale in children with anorectal malformations. J Pediatr Surg 42:1015–1021. https://doi.org/10.1016/j.jpedsurg.2007.01.070
van der Jagt PKN, Dik P, Froeling M, Kwee TC, Nievelstein RAJ, ten Haken B et al (2012) Architectural configuration and microstructural properties of the sacral plexus: a diffusion tensor MRI and fiber tractography study. Neuroimage 62:1792–1799. https://doi.org/10.1016/j.neuroimage.2012.06.001
Rigueros Springford L, Connor MJ, Jones K, Kapetanakis VV, Giuliani S (2016) Prevalence of active long-term problems in patients with anorectal malformations: a systematic review. Dis Colon Rectum 59:570–580. https://doi.org/10.1097/DCR.0000000000000576
Jeon T, Fung MM, Koch KM, Tan ET, Sneag DB (2018) Peripheral nerve diffusion tensor imaging: overview, pitfalls, and future directions. J Magn Reson Imaging 47:1171–1189. https://doi.org/10.1002/jmri.25876
Noguerol TM, Barousse R, Socolovsky M, Luna A (2017) Quantitative magnetic resonance (MR) neurography for evaluation of peripheral nerves and plexus injuries. Quant Imaging Med Surg 7:398–421. https://doi.org/10.21037/qims.2017.08.01
Holschneider A, Koebke J, Meier-Ruge W, Land N, Jesch N, Pfrommer W (2001) Pathophysiology of chronic constipation in anorectal malformations. Eur J Pediatr Surg 11:305–310
Muller C, Virzi A, Marret J-B, Mille E, Cretolle C, Gori P et al (2018) Analysis of sacral plexus anatomy using MRI based neurotractography, according to spinal dysraphism, sacral anomaly and type of anorectal malformation. In: 19th European congress pediatric surgery, Paris, 2018, p 2
Borg H, Holmdahl G, Olsson I, Wiklund LM, Sillén U (2009) Impact of spinal cord malformation on bladder function in children with anorectal malformations. J Pediatr Surg 44:1778–1785. https://doi.org/10.1016/j.jpedsurg.2009.03.001
Fuchs ME, Halleran DR, Shin YJ, Sebastião Y, Weaver L, Ahmad H et al (2020) Anatomic factors predict urinary continence in patient with anorectal malformation. J Pediatr Urol 16:545.e1-545.e7. https://doi.org/10.1016/j.jpurol.2020.06.011
Vilanova-Sanchez A, Reck CA, Sebastião YV, Fuchs M, Halleran DR, Weaver L et al (2018) Can sacral development as a marker for caudal regression help identify associated urologic anomalies in patients with anorectal malformation? J Pediatr Surg 53:2178–2182. https://doi.org/10.1016/j.jpedsurg.2018.03.018
Torre M, Martucciello G, Jasonni V (2001) Sacral development in anorectal malformations and in normal population. Pediatr Radiol 31:858–862. https://doi.org/10.1007/s002470100006
Funding
This work was supported by Aliye Uster Foundation (Izmir, Turkey) research scholarship. This is an independent organization funding educational and research activities in Ege University. The authors have no conflict of interest regarding the study.
Author information
Authors and Affiliations
Contributions
All the authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Sibel Tiryaki, Cenk Eraslan and Ulgen Celtik. The first draft of the manuscript was written by Sibel Tiryaki, and all the authors commented on previous versions of the manuscript. All the authors read and approved the final manuscript.
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tiryaki, S., Celtik, U., Eraslan, C. et al. Diffusion tensor imaging in anorectal malformations: a pilot study for the evaluation of lumbosacral plexus. Pediatr Surg Int 38, 609–616 (2022). https://doi.org/10.1007/s00383-022-05077-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-022-05077-3