Abstract
Purpose
The VICI-trial reported that in patients with congenital diaphragmatic hernia (CDH), mortality or bronchopulmonary dysplasia (BPD) were equivalent using conventional mechanical ventilation (CMV) and high-frequency oscillatory ventilation. The purpose of this study was to determine if the mode of ventilation at the time of CDH repair affected mortality or oxygen dependence at 28 days.
Methods
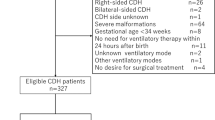
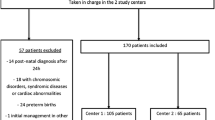
We performed a retrospective cohort study of infants born wih CDH from 1991 to 2015. A generalized linear model was applied to the data using a propensity score analysis.
Results
Eighty patients met the inclusion criteria; at the time of surgery 39 (48.8%) patients were on HFV and 41 (51.3%) patients were on CMV. In the HFV group, 16 (47.1%) patients remained oxygen dependent and there were 5 (12.8%) deaths at 28 days. In the CMV group, 5 (12.2%) patients remained oxygen dependent at 28 days but none had died. The base model demonstrated that the HFV group had increased rates of oxygen dependence [OR = 6.40 (2.13, 22.2), p = 0.002]. However, after propensity score analysis, we found no difference between HFV and CMV.
Conclusion
Our study suggests that in infants with CDH, there is no significant difference between HFV and CMV in oxygen dependency or death.

Similar content being viewed by others
References
de Buys Roessingh AS, Dinh-Xuan AT (2009) Congenital diaphragmatic hernia: current status and review of the literature. Eur J Pediatr 168(4):393–406. https://doi.org/10.1007/s00431-008-0904-x
Skari H, Bjornland K, Haugen G, Egeland T, Emblem R (2000) Congenital diaphragmatic hernia: a meta-analysis of mortality factors. J Pediatr Surg 35(8):1187–1197. https://doi.org/10.1053/jpsu.2000.8725
Balayla J, Abenhaim HA (2014) Incidence, predictors and outcomes of congenital diaphragmatic hernia: a population-based study of 32 million births in the United States. J Matern Neonatal Med 27(14):1438–1444. https://doi.org/10.3109/14767058.2013.858691
Logan JW, Cotten CM, Goldberg RN, Clark RH (2007) Mechanical ventilation strategies in the management of congenital diaphragmatic hernia. Semin Pediatr Surg 16(2):115–125. https://doi.org/10.1053/j.sempedsurg.2007.01.006
Kuluz MA, Smith PB, Mears SP et al (2010) Preliminary observations of the use of high-frequency jet ventilation as rescue therapy in infants with congenital diaphragmatic hernia. J Pediatr Surg 45(4):698–702. https://doi.org/10.1016/j.jpedsurg.2009.07.025
Keszler M, Modanlou HD, Brudno DS et al (1997) Multicenter controlled clinical trial of high-frequency jet ventilation in preterm infants with uncomplicated respiratory distress syndrome. Pediatrics 100(4):593–599. https://doi.org/10.1542/peds.100.4.593
Migliazza L, Bellan C, Alberti D et al (2007) Retrospective study of 111 cases of congenital diaphragmatic hernia treated with early high-frequency oscillatory ventilation and presurgical stabilization. J Pediatr Surg 42:1526–1532. https://doi.org/10.1016/j.jpedsurg.2007.04.015
Somaschini M, Locatelli G, Salvoni L, Bellan C, Colombo A (1999) Impact of new treatments for respiratory failure on outcome of infants with congenital diaphragmatic hernia. Eur J Pediatr 158(10):780–784. https://doi.org/10.1007/s004310051203
Ng GYT, Derry C, Marston L, Choudhury M, Holmes K, Calvert SA (2008) Reduction in ventilator-induced lung injury improves outcome in congenital diaphragmatic hernia? Pediatr Surg Int 24(2):145–150. https://doi.org/10.1007/s00383-007-2051-2
Cacciari A, Ruggeri G, Mordenti M et al (2001) High-frequency oscillatory ventilation versus conventional mechanical ventilation in congenital diaphragmatic hernia. Eur J Pediatr Surg 11(1):3–7. https://doi.org/10.1055/s-2001-12204
Miguet D, Claris O, Lapillonne A, Bakr A, Chappuis J-P, Salle BL (1994) Preoperative stabilization using high-frequency oscillatory ventilation in the management of congenital diaphragmatic hernia. Crit Care Med. https://doi.org/10.1097/00003246-199422091-00008(22(SUPPL.):S77-S82)
Reyes C, Chang LK, Waffarn F, Mir H, Warden MJ, Sills J (1998) Delayed repair of congenital diaphragmatic hernia with early high- frequency oscillatory ventilation during preoperative stabilization. J Pediatr Surg 33:1010–1016. https://doi.org/10.1016/S0022-3468(98)90523-1(W.B. Saunders)
van den Hout L, Reiss I, Felix JF et al (2010) Risk factors for chronic lung disease and mortality in newborns with congenital diaphragmatic hernia. Neonatology 98(4):370–380. https://doi.org/10.1159/000316974
Snoek KG, Capolupo I, Van Rosmalen J et al (2016) Conventional mechanical ventilation versus high-frequency oscillatory ventilation for congenital diaphragmatic hernia. A randomized clinical trial (The VICI-trial). Ann Surg 263(5):867–874. https://doi.org/10.1097/SLA.0000000000001533
Tsao KJ, Lally KP (2008) The congenital diaphragmatic hernia study group: a voluntary international registry. Semin Pediatr Surg 17(2):90–97. https://doi.org/10.1053/j.sempedsurg.2008.02.004
Austin PC (2011) An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivar Behav Res 46(3):399–424. https://doi.org/10.1080/00273171.2011.568786
Lally KP, Lally PA, Lasky RE et al (2007) Defect size determines survival in infants with congenital diaphragmatic hernia. Pediatrics 120(3):e651–e657. https://doi.org/10.1542/peds.2006-3040
Congenital Diaphragmatic Hernia Study Group (2001) Estimating disease severity of congenital diaphragmatic hernia in the first 5 minutes of life. J Pediatr Surg 36(1):141–145. https://doi.org/10.1053/JPSU.2001.20032
Rosenbaum PR, Rubin DB (1984) Reducing bias in observational studies using subclassification on the propensity score. J Am Stat Assoc 79(387):516–524
D'Agostino RB Jr (1998) Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med 17(19):2265–2281
Acknowledgements
This work was supported by the DEVOTION Network and the Children’s Hospital Research Institute of Manitoba; Dr. Richard Keijzer is the Thorlakson Chair in Surgical Research for the Department of Surgery and the University of Manitoba. Richard Keijzer (conceptualization, funding acquisition, resources, supervision, writing—review and editing).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All of the following authors—Matthew Levesque, Gabrielle Derraugh, Daryl Schantz, Melanie I. Morris, Anna Shawyer, Suyin A. Lum Min, Richard Keijzer—have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Derraugh, G., Levesque, M., Schantz, D. et al. High-frequency vs. conventional ventilation at the time of CDH repair is not associated with higher mortality and oxygen dependency: a retrospective cohort study. Pediatr Surg Int 36, 1275–1280 (2020). https://doi.org/10.1007/s00383-020-04740-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-020-04740-x