Abstract
Aim
To analyze the impact of counseling on antenatal congenital surgical anomalies (ACSA).
Methods
Cases presenting with ACSA for fetal counseling and those presenting in post-natal period following diagnosis of ACSA (PACSA) for surgical opinion were analyzed for spectrum, presentation and outcome.
Results
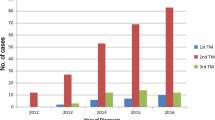
117 cases including ACSA(68);PACSA(49) were analyzed. Gestational age at diagnosis of ACSA;PACSA was 17–37;17–39 weeks (median 24;32 weeks). Diagnoses in ACSA;PACSA included urological (26;31), neurological (10;5), congenital diaphragmatic hernia (CDH)(5;1), gastrointestinal (5;5), lung and chest anomalies (5;1), intraabdominal cysts (4;1), abdominal wall defects (4;0), tumors (3;3), limb anomaly (1;1), esophageal atresia (1;1), conjoint twins (1;0), hepatomegaly (1;0), and major cardiac anomalies (2;0). Two antenatal interventions were done for ACSA; vesicoamniotic shunt and amnioinfusion for oligohydramnios. 17;24 ACSA;PACSA required early surgical intervention in post-natal period. Nine ACSA underwent medical termination of pregnancy and 4 had intrauterine demise. Nine ACSA babies died including two CDH, one gastroschisis, one duodenal atresia, one conjoint twins, one megacystitis with motility disorder and three posterior urethral valves. All PACSA babies survived.
Conclusion
Fetal counseling for CSA portrays true outcome of ACSA with 32.3% (22/68) mortality versus 0% for PACSA due to selection bias. However, fetal counseling ensures optimal perinatal care.








Similar content being viewed by others
References
Sixty-third World Health Assembly report on birth defects (2010). apps.who.int/gb/ebwha/pdf_files/WHA63/A63_10-en.pd
World Health Organization (2008) The global burden of disease: 2004 update. World Health Organization, Geneva
Crombleholme TM, D’Alton M, Cendron M et al (1996) Prenatal diagnosis and the pediatric surgeon: the impact of prenatal consultation on perinatal management. J Pediatr Surg 31:156–162 (discussion 162–163)
Dibbins AW, Curci MR, McCrann DJ Jr (1985) Prenatal diagnosis of congenital anomalies requiring surgical correction. Implications for the future. Am J Surg 149:528–533
Wilcox DT, Karamanoukian HL, Glick PL (1993) Antenatal diagnosis of pediatric surgical anomalies. Counseling the family. Pediatr Clin North Am 40:1273–1287
Benn PA, Egan JF, Fang M, Smith-Bindman R (2004) Changes in the utilization of prenatal diagnosis. Obstet Gynecol 103:1255–1260
EUROCAT European survellience of congenital anomalies. http://www.eurocat-network.eu/. Accessed 26 Sept 2016
The Congenital Malformations Registry of the New York State, Department of Health. www.health.ny.gov › Diseases and Conditions. Accessed 26 Sept 2016
Fetal Care Research Foundation—Birth Defects Registry of India (BDRI)—a ‘Saving Babies’ Project. http://www.fcrf.org.in/bdri_abus.asp. Accessed 26 Sept 2016
Tibrewal NS, Pai PM (1974) Congenital malformations in newborn period. Indian Pediatr 11:403–407
Kulshreshta R, Nath LM, Upadhyay P (1983) Congenital malformations in live born infants in a rural community. Indian Pediatr 20:45–49
Verma IC, Mathews AR (1983) Congenital malformations in India. In: Satyavati GV (ed) Peoples of India: some genetic aspects. Indian Council of Medical Research, New Delhi, p 70
Verma M, Chhatwal J, Singh D (1991) Congenital malformations-a retrospective study of 10,000 cases. Indian Pediatr 28:245–252
Chaturvedi P, Banerjee KS (1993) An epidemiological study of congenital malformations in newborn. Indian J Pediatr 60:645
Swain S, Agrawal A, Bhatia BD (1994) Congenital malformations at birth. Indian Pediatr 31:1187–1191
Kumar V, Singh AJ, Marwaha RK (1994) An epidemiological study of congenital malformations in rural children. Indian Pediatr 31:909–914
Bhat BV, Babu L (1998) Congenital malformations at birth–a prospective study from south India. Indian J Pediatr 65:873–881
Grover N (2000) Congenital malformations in Shimla. Indian J Pediatr 67:249–251
Datta V, Chaturvedi P (2000) Congenital malformations in rural Maharashtra. Indian Pediatr 37:998–1001
Dutta HK, Bhattacharyya NC, Sarma JN, Giriraj K (2010) Congenital malformations in Assam. J Indian Assoc Pediatr Surg 15:53–55
Gupta DK, Sharma S, Gupta M (2010) Outcome of antenatally referred congenital surgical anomalies—a pediatric surgeon’s perspective. J Pediatr Surg Spec 4:1–9
Pineda-Del Villar L, Martínez-Basalo MC, Delgado W, Prieto-Carrasquero M, Villasmil Y (1994) Epidemiology of congenital malformations at the Hospital Pedro García Clara, Ciudad Ojeda. Venezuela. Invest Clin 35:19–34
Tayebi N, Yazdani K, Naghshin N (2010) The prevalence of congenital malformations and its correlation with consanguineous marriages. OMJ 25:37–40
Penchaszadeh VB (2002) Preventing congenital anomalies in developing countries. Community Genet 5:61–69
Romero R (1993) Routine obstetric ultrasound. Ultrasound Obstet Gynecol 3:303–307
Crane JP, LeFevre ML, Winborn RC, Evans JK, Ewingman BG, Bain RP et al (1994) RADIUS Study Group. A randomised trial of prenatal ultrasonographic screening: impact on the detection, management, and outcome of anomalous fetuses. Am J Obstet Gynecol 171:392–399
Levine D, Barnes PD, Madsen JR, Abbot J, Tejas Meta T, Edelman R (1999) Central nervous system abnormalities assessed with magnetic resonance. Obstet Gynecol 94:1011–1019
Todros T, Capuzzo E, Gaglioti P (2001) Prenatal diagnosis of congenital anomalies. Images Paediatr Cardiol 3:3–18
Grandjean H, Larroque D, Levi S (1999) Eurofetus Study Group. The performance of routine ultrasonographic screening of pregnancies in the Eurofetus Study. Am J Obstet Gynecol 181:446–454
Johnson P, Sebire NJ, Snijders RJM, Tunkel S, Nicolaides KH (1997) Ultrasound screening for anencephaly at 10–14 weeks of gestation. Ultrasound Obstet Gynecol 9:14–16
Chitty LS, Pandya PP (1997) Ultrasound screening for fetal abnormalities in the first trimester. Prenat Diagn 17:1269–1281
Pilu G, Perolo A, Falco P, Visentin A, Gabrielli G, Bovicelli L (2000) Ultrasound of the central nervous system. Curr Opin Obstet Gynecol 12:93–103
Sebire NJ, Noble PL, Thorpe-Beeston JG, Snijders RJ, Nicolaides K (1997) Presence of the ‘lemon’ sign in fetuses with spina bifida at the 10-14-week scan. Ultrasound Obstet Gynecol 10:403–407
Gembruch U (1997) Prenatal diagnosis of congenital heart disease. Prenat Diagn 17:1283–1297
Todros T, Faggiano F, Chiappa E, Gaglioti P, Mitola B, Sciarrone A (1997) Gruppo piemontese for prenatal screening of congenital heart disease. Accuracy of routine ultrasonography in screening heart disease prenatally. Prenat Diagn 17:901–906
Fesslova V, Nava S, Villa L (1999) Fetal Cardiology Study Group of the Italian Society of Pediatric Cardiology. Evolution and long term outcome in cases with fetal diagnosis of congenital heart disease: Italian multicentre study. Heart 82:549–599
Allan LD, Sharland GK, Milburn A, Lockhart SM, Groves AMM, Anderson RH et al (1994) Prospective diagnosis of 1,006 consecutive cases of congenital heart disease in the fetus. J Am Coll Cardiol 23:1452–1458
Raymond FL, Simpson JM, Sharland GK, Mackie Ogilvie CM (1997) Fetal echocardiography as a predictor of chromosomal abnormality. Lancet 350:930
Yates R (1999) Fetal cardiac abnormalities and their association with aneuploidy. Prenat Diagn 19:563–566
Lynema S, Fifer CG, Laventhal NT (2016) Perinatal decision making for preterm infants with congenital heart disease: determinable risk factors for mortality. Pediatr Cardiol 37:938–945
Todros T (2000) Prenatal diagnosis and management of fetal cardiovascular malformations. Curr Opin Obstet Gynecol 12:87–92
Kalter H, Warkany J (1983) Congenital malformations (first of two parts). N Engl J Med 308:424–431
Kalter H, Warkany J (1983) Congenital malformations (second of two parts). N Engl J Med 308:491–497
Neilson JP (2000). Ultrasound for fetal assessment in early pregnancy. The cochrane database of systematic reviews. 2
Zimmer EZ, Avraham Z, Sujoy P, Goldstein I, Bronshtein M (1997) The influence of prenatal ultrasound on the prevalence of congenital anomalies at birth. Prenat Diagn 17:623–628
Bull C (1999) Current and potential impact of fetal diagnosis on prevalence and spectrum of serious congenital heart disease at term in the UK. Lancet 354:1242–1247
Parilla BV, Leeth EA, Kambich MP, Chilis P, MacGregor SN (2003) Antenatal detection of skeletal dysplasias. J Ultrasound Med. 22:255–258 (quiz 259–261)
Tonni G, Granese R, Martins Santana EF, Parise Filho JP, Bottura I, Borges Peixoto A et al (2016) Prenatally diagnosed fetal tumors of the head and neck: a systematic review with antenatal and postnatal outcomes over the past 20 years. J Perinat Med. doi:10.1515/jpm-2016-0074
Shalaby H, Hemida R, Nabil H, Ibrahim M (2016) Types and outcome of fetal urinary anomalies in low resource setting countries: a retrospective study. J Obstet Gynaecol India 66:316–320
Bondagji NS (2014) Antenatal diagnosis, prevalence and outcome of congenital anomalies of the kidney and urinary tract in Saudi Arabia. Urol Ann. 6:36–40
Andrés-Jensen L, Jørgensen FS, Thorup J, Flachs J, Madsen JL, Maroun LL et al (2016) The outcome of antenatal ultrasound diagnosed anomalies of the kidney and urinary tract in a large Danish birth cohort. Arch Dis Child 101:819–824
Policiano C, Djokovic D, Carvalho R, Monteiro C, Melo MA, Graça LM (2015) Ultrasound antenatal detection of urinary tract anomalies in the last decade: outcome and prognosis. J Matern Fetal Neonatal Med 28:959–963
Altokhais T, Soomro MA, Gado A, Albassam A (2016) Bedside neonatal intensive care unit correction of congenital diaphragmatic hernia: is repair without compromise? Am J Perinatol 33:861–865
Fievet L, Natale C, D’Journo XB, Coze S, Dubus JC, Guys JM et al (2015) Congenital pulmonary airway malformation and sequestration: two standpoints for a single condition. J Minim Access Surg. 11:129–133
Lamquami S, Mamouni N, Errarhay S, Bouchikhi C, Banani A (2015) Antenatal diagnosis of isolated omphalocele. Pan Afr Med J. 21:233
Tarcă E, Aprodu S (2014) Past and present in omphalocele treatment in Romania. Chir (Bucur) 109:507–513
Ţarcă E, Ciongradi I, Aprodu SG (2015) Birth weight, compromised bowel and sepsis are the main variables significantly influencing outcome in gastroschisis. Chir (Bucur) 110:151–156
Lepigeon K, Van Mieghem T, Vasseur Maurer S, Giannoni E, Baud D (2014) Gastroschisis—what should be told to parents? Prenat Diagn 34:316–326
Okur MH, Arslan MS, Arslan S, Aydogdu B, Türkçü G, Goya C et al (2014) Gastrointestinal tract duplications in children. Eur Rev Med Pharmacol Sci 18:1507–1512
Ballehaninna UK, Nguyen T, Burjonrappa SC (2013) Laparoscopic resection of antenatally identified duodenal duplication cyst. JSLS 17:454–458
Agrawal A, Sampley S (2014) Spinal dysraphism: a challenge continued to be faced by neurosurgeons in developing countries. Asian J Neurosurg 9:68–71
McClure EM, Saleem S, Goudar SS, Moore JL, Garces A, Esamai F et al (2015) Stillbirth rates in low-middle income countries 2010–2013: a population-based, multi-country study from the Global Network. Reprod Health 12(Suppl 2):S7
Nayak SS, Shukla A, Girisha KM (2015) Anomalies associated with single umbilical artery at perinatal autopsy. Indian Pediatr 52:73–74
Morris JK, Garne E, Wellesley D, Addor MC, Arriola L, Barisic I et al (2014) Major congenital anomalies in babies born with Down syndrome: a EUROCAT population-based registry study. Am J Med Genet A 164A:2979–2986
Lakhoo K (2012) Fetal counselling for surgical conditions. Early Hum Dev. 88:9–13
Acknowledgements
This work is done under a project sponsored by the Department of Biotechnology, Government of India. Reference BT/PR9572/MED/97/210/2013. Website: http://birthdefect.in/.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sharma, S., Bhanot, R., Deka, D. et al. Impact of fetal counseling on outcome of antenatal congenital surgical anomalies. Pediatr Surg Int 33, 203–212 (2017). https://doi.org/10.1007/s00383-016-4015-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-016-4015-x