Abstract
Background
Nitrous oxide’s safety and efficacy for minor procedures is an alternative to general anesthesia, complex sedation protocols, or local anesthetic alone.
Methods
A retrospective review of prospectively-collected data (2000–2012) identified 1,058 children who received single-agent nitrous oxide for minor surgery.
Results
Children (n = 1,058, male 42 %, female 58 %) aged 1–23 years (mean = 9.8 + 5.1 years) were identified. Only nine children (0.9 %) fasted. ASA status was I–II in 1,053 (99.5 %) of patients; five (0.5 %) had an ASA III. There were no major complications (desaturation, emergency admission, apnea, airway obstruction, bradycardia) or aborted procedures. Minor complications occurred in 1.8 %; there was no association between these complications and ASA, fasting status or maximum nitrous oxide percentage administered (all p > 0.05). Post-operatively, 98 % of patients denied getting an injection. Eighty-two percent reported mild or no procedural pain.
Conclusion
This is the longest reported study using non-anesthesiologist-administered nitrous oxide as a single-agent for minor surgical procedures. The technique provides safe sedation and excellent amnesia, allowing pain and anxiety-reduced surgery with no fasting or postoperative monitoring.


Similar content being viewed by others
References
Committee on Psychosocial Aspects of Child and Family Health and Task Force on Pain in Infants, Children, and Adolescents (2001) The assessment and management of acute pain in infants, children, and adolescents. Pediatrics 108:793–797
Taylor EM, Boyer K, Campbell FA (2008) Pain in hospitalized children: a prospective crosssectional survey of pain prevalence, intensity, assessment and management in a Canadian pediatric teaching hospital. Pain Res Manage 13:25–32
Kennedy RM, Luhmann J, Zempsky WT (2008) Clinical implications of unmanaged needle-insertion pain and distress in children. Pediatrics 122:S130–S133
Uman L, Chambers C, McGrath P, Kisely S (2008) A systematic review of randomized controlled trial examining psychological interventions for needle-related procedural pain and distress in children and adolescents: an abbreviated Cochrane review. J Pediatr Psychol 33(8):842–854. doi:10.1093/jpepsy/jsn031
Blount RL, Louiselle KA (2009) Behavioural assessment of pediatric pain. Pain Res Manage 14:47–52
Sohn VY, Zenger D, Steel SR (2012) Pain management in the pediatric surgical patient. Surg Clin North Am 92:471–485, vii. doi:10.1016/j.suc.2012.03.002
Orrett E, Hertz M (2012) Anxiety control in the dental patient. Dent Clin N Am 56:1–16
Hla KT, Hegarty M, Russell P, Drake-Brockman TF, Ramgolan A, von Ungern-Sternberg BS (2014) Perception of pediatric pain: a comparison of postoperative pain assessments between child, parent, nurse, and independent observer. Paediatr Anaesth. doi:10.1111/pan.12484
Dvorkin R, Bair J, Patel H, Glantz S, Yens DP, Rosalia A, Marguilies J (2014) Is fever treated more promptly than pain in the pediatric emergency department? J Emerg Med 46:327–334. doi:10.1016/j.jemermed.2013.08.063
Avansino JR, Peters L, Stockfish SL, Walco GA (2013) A paradigm shift to balance safety and quality in pediatric pain management. Pediatrics 131:e921–e926
Connors J, Cravero J, Kost S, La Violette D, Lowrie L, Scherrer P. (2013) Great expectations—defining quality in pediatric sedation: outcomes of a multidisciplinary consensus conference. J Healthc Qual 1–13
Evered LM (2003) Procedural sedation and analgesia for pediatric patients in the emergency department. Paediatr Child Health 8:503–507
Becker DE, Rosenberg M (2008) Nitrous oxide and the inhalation anesthetics. Anesth Prog 55:124–131
American Academy on Pediatrics; American Academy on Pediatric Dentistry (2008–2009) Guideline for monitoring and management of pediatric patients during and after sedation for diagnostic and therapeutic procedures. Pediatr Dent 30(7 Suppl):143–59
Alkire MT, Gorski LA (2004) Relative amnesic potency of five inhalation anesthetics follows the Meyer-Overton rule. Anesthesiology 101:417–429
Zier JL, Liu M (2001) Safety of high-concentration nitrous oxide by nasal mask for pediatric procedural sedation: experience with 7,802 cases. Pediatr Emerg Care 27:1107–1112
American Academy of Pediatric Dentistry Council on Clinical Affairs (2008–2009) Guideline on appropriate use of nitrous oxide for pediatric dental patients. Pediatr Dent 30(7 Suppl):140–2
Kupietzky A, Tal E, Shapira J, Ram D (2008) Fasting state and episodes of vomiting in children receiving nitrous oxide for dental treatment. Pediatr Dent 30:414–419
Roberts GJ, Wignall BK (1982) Efficacy of the laryngeal reflex during oxygen nitrous oxide sedation (relative analgesia). Br J Anesth 54:1277–1281
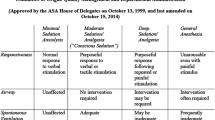
American Society of Anesthesiologists Task Force on Sedation and Analgesia by Non-Anesthesiologists (2002) Practice guidelines for sedation and analgesia by non-anesthesiologists. Anesthesiology 96:1004–1017
Babl FE, Oakley E, Puspitadewi A, Sharwood LN (2008) Limited analgesic efficacy of nitrous oxide for painful procedures in children. Emerg Med J 25:717–721
Zier JL, Drake GJ, McCormick PC, Clinch KM, Cornfield DN (2007) Case-series of nurse-administered nitrous oxide for urinary catheterization. Anesth Analg 104:876–879
Zier JL, Tarrago R, Liu M (2010) Level of sedation with nitrous oxide for pediatric medical procedures. Anesth Analg 110:1399–1405
Burnweit C, Diana-Zerpa JA, Nahmad MH, Lankau CA, Weinberger M, Malvezzi L, Smith L, Shapiro T, Thayer K (2004) Nitrous oxide analgesia for minor pediatric surgical procedures: an effective alternative to conscious sedation? J Pediatr Surg 39:495–499
Annequin D, Carbajal R, Chauvin P, Gall O, Tourniaire B, Murat I (2000) Fixed 50% nitrous oxide mixture for pain procedures: a French survey. Pediatrics 105:E47
Babl FE, Oakley E, Seaman C, Barnett P, Sharwood LN (2008) High-concentration nitrous oxide for procedural sedation in children: adverse events and depth of sedation. Pediatrics 121:e528
Bar-Mier E, Zaslansky R, Regev E, Keidan I, Orenstein A, Winkler E (2006) Nitrous oxide administered by the plastic surgeon for the repair of facial lacerations in children in the emergency room. Plast Reconstr Surg 117:1571–1575
Denman WT, Tuason PM, Ahmed MI, Brennen LM, Cepeda MS, Carr DB (2007) The PediSedate® device, a novel approach to pediatric sedation that provides distraction and inhaled nitrous oxide: clinical evaluation in a large case series. Pediatr Anesth 17:162–166
Frampton A, Browne GJ, Lam LT, Cooper MG, Lane LG (2003) Nurse administered relative analgesia using high concentration nitrous oxide to facilitate minor procedures in children in an emergency department. Emerg Med J 20:410–413
Gómez B, Capagé S, Benito FJ, Landa J, Fernández Y, Luaces C, Serrano O, Freijó MC, May ME, Aldecoa V, Grupo de Trabajo de Anelgesia y Sedación de la SEUP (2011) Efectividad y seguridad del uso de óxido nitroso para sedoanalgesia en urgencias. An Pediatr (Barc) 75:96–102
Onody P, Gil P, Hennequin M (2006) Safety inhalation of a 50% nitrous oxide/oxygen premix: a prospective survey of 35,828 administrations. Drug Saf 29:633–640
Reinoso-Barbeiro F, Pascual-Pascual SI, de Lucas R, García S, Billoët C, Duquenne V, Onody P (2011) Equimolar nitrous oxide/oxygen versus placebo for procedural pain in children: a randomized trial. Pediatrics 127:e1464–e1470
Uziel Y, Chanick G, Rothschild M, Tauber T, Press J, Harel L, Hashkes PJ (2008) Nitrous oxide for intra-articular injection in juvenile idiopathic arthritis. Pediatr Rheumatol 6:1. doi:10.1186/1546-0096-6-1
Clark, Brunick AL (2008) Handbook of nitrous oxide and oxygen sedation, vol 3. Mosby Elsevier, St. Louis
Selzer RR, Rosenblatt DS, Laxova R, Hogan R (2003) Adverse efect of nitrous oxide in a child with 5,10-methylenetetrahydrofolate reductase deficiency. N Engl J Med 349:45–50
Malviya S, Voepel-Lewis T, Tait AR, Merkel S, Tremper K, Naughton N (2002) Depth of sedation in children undergoing computed tomography: validity and reliability of the University of Michigan Sedation Scale (UMSS). Br J Anesth 88:241–245
Wong DL, Baker CM (1988) Pain in children: comparison of assessment scales. Pediatr Nurs 14:9–17
Davis J, Alkhoury F, Burnweit C (2014) Surgical and anesthetic considerations in histrelin capsule implantation for the treatment of precocious puberty. J Pediatr Surg 49:807–810
Sahyoun C, Kraus B (2012) Clinical implications of pharmacokinetics and pharmacodynamics of procedural sedation agents in children. Curr Opin Pediatr 24:225–232
Zier JL, Doescher JS (2010) Seizures temporally associated with nitrous oxide administration for pediatric procedural sedation. J Child Neuro 25:1517–1520
Cravero JP, Beach ML, Blike GT, Gallagher SM, Hertzog JH, Pediatric Sedation Research Consortium (2009) The incidence and nature of adverse events during pediatric sedation/anesthesia with propofol for procedures outside the operating room: a report from the Pediatric Sedation Research Consortium. Anesth Analg 108:795–804
Conflict of interest
The authors have no conflict of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pasarón, R., Burnweit, C., Zerpa, J. et al. Nitrous oxide procedural sedation in non-fasting pediatric patients undergoing minor surgery: a 12-year experience with 1,058 patients. Pediatr Surg Int 31, 173–180 (2015). https://doi.org/10.1007/s00383-014-3608-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-014-3608-5