Abstract
Purpose
Generally, open portoenterostomy (PE) involves a wide extended anastomosis and all sutures are deep [extended PE (EP)]. In contrast, the anastomosis in Kasai’s PE (KP), our modified open Kasai PE (MK), and our laparoscopic modified Kasai PE (lapMK) involve shallow suturing, especially at the 2 and 10 o’clock positions where the right and left bile ducts would be normally. We compared outcomes of 36 consecutive biliary atresia (BA) patients treated by three types of PE at a single institution during the period 2005–2014; EP (n = 13), MK (n = 11), and lapMK (n = 12).
Methods
We compared age at PE, time taken to become jaundice-free (total bilirubin ≤1.2 mg/dL; JF time), proportion of JF subjects [JF ratio (JFR)], steroid dosage, incidence of cholangitis, postoperative liver function and CRP, presence of hypersplenism, requirement for liver transplantation (LTx), and JF survival with the native liver (JF+NL) as indicators of outcome.
Results
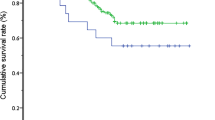
Patient demographics, steroid dosage, JF time, incidence of cholangitis, presence of hypersplenism, operating time, blood loss and postoperative biochemistry were similar for all groups. However, JFR was significantly higher for lapMK (100 %) versus EP (46.2 %) (p < 0.05), but not for MK (81.8 %) versus EP. Kaplan–Meier analysis showed survival with NL was significantly higher for lapMK (10/12: 83.3 %: JF in 9; not JF in 1) and MK (9/11: 81.8 %: JF in all) versus EP (3/13: 23.1 %: JF in all) (p < 0.05, respectively), but not for lapMK versus MK. JF+NL in both lapMK (9/12: 75.0 %) and MK (9/11: 81.8 %) were significantly higher compared with EP (3/13: 23.1 %) (p < 0.05, respectively). Intraperitoneal adhesions were less pronounced at LTx in lapMK compared with MK or EP.
Conclusions
This study would suggest that depth of suturing during PE would appear to influence post-PE outcome. LapMK should be reconsidered as a valid treatment option for BA.



Similar content being viewed by others
References
Kasai M, Suzuki S (1959) A new operation for non-correctable biliary atresia: hepatic portoenterostomy. Shujutu 13:733–779
Kasai M (1974) Treatment of biliary atresia with special reference to hepatic portoenterostomy and its modification. Prog Pediatr Surg 6:5–52
Karrer FM, Pence JC (2003) Biliary atresia and choledochal cyst. In: Ziegler MM, Azizkhan RG, Weber TR (eds) Operative pediatric surgery, 5th edn. McGraw-Hill, New York, pp 775–787
Esteves E, Clemente NE, Ottaiano NM et al (2002) Laparoscopic Kasai Portenterostomy for biliary atresia. Pediatr Surg Int 18:737–740
Davenport M, Ure BM, Petersen C (2007) Surgery for biliary atresia—is there a European consensus? Eur J Pediatr Surg 17:180–183
Wong KK, Chung PH, Chan KL et al (2008) Should open Kasai portoenterostomy be performed for biliary atresia in the era of laparoscopy? Pediatr Surg Int 24:931–933
Ure BM, Kuebler JF, Schukfeh N et al (2011) Survival with the native liver after laparoscopic versus conventional Kasai portoenterostomy in infants with biliary atresia: a prospective trial. Ann Surg 253:826–830
Bax NMA, Georgeson K (2007) Biliary atresia panel session. In: Presentation at the 16th annual congress of the International Pediatric Endosurgery Group, Buenos Aires, Argentina, 6–9 September
Nakamura H, Koga H, Wada M et al (2012) Reappraising the portoenterostomy procedure according to sound physiologic/anatomic principles enhances postoperative jaundice clearance in biliary atresia. Pediatr Surg Int 28:205–209
Koga H, Miyano G, Takahashi T et al (2011) Laparoscopic portoenterostomy for uncorrectable biliary atresia using Kasai’s original technique. J Laparoendosc Adv Surg Tech A 21:291–294
Nakamura H, Koga H, Miyano G et al. (2013) Gastrointestinal and hepatobiliary scientific session. In: Presentation at the 22nd annual congress of the International Pediatric Endosurgery Group, Beijing, China, 17–22 June
Davenport M (2012) Biliary atresia: clinical aspects. Semin Pediatr Surg 21:175–184
Ohi R (2001) Surgery for biliary atresia. Liver 21:175–182
Ando H, Seo T, Ito F et al (1997) A new hepatic portoenterostomy with division of the ligamentum venosum for treatment of biliary atresia. J Pediatr Surg 32:1552–1554
Endo M, Katsumata K, Yokoyama Y et al (1983) Extended dissection of the porta hepatis and creation of an intussuscepted ileocolic conduit for biliary atresia. J Pediatr Surg 18:784–793
Kobayashi H, Yamataka A, Urao M et al (2006) Innovative modification of the hepatic portoenterostomy. Our experience of treating biliary atresia. J Pediatr Surg 41:E19–E22
Ohi R (1999) Portoenterostomy for Biliary atresia. Japan surgical society video library no. 99-05
Kasai M (1978) Surgery for biliary atresia. Japan surgical society video library no. 78-07
Altman RP, Buchmiller TL (2006) The jaundiced infant: biliary atresia. In: Grosfeld JL, O’Neill JA, Coran AG et al (eds) Pediatric surgery, 6th edn. Mosby Elsevier, Philadelphia, pp 1603–1616
Nio M, Sasaki H, Wada M et al (2010) The validity of currently performed procedures for treating biliary atresia based on postsurgical outcome at our center (abstract in Japanese). J Jpn Soc Pediatr Surg 46:430
Yamataka A, Koga H, Miyano G et al (2009) Laparoscopic portoenterostomy for biliary atresia: our experience (Abstract in Japanese). In: Presentation at the 36th annual congress of the Japan biliary atresia society, Yokohama, Japan, 12 December
Martinez-Ferro M, Esteves E, Laje P et al (2005) Laparoscopic treatment of biliary atresia and choledochal cyst. Semin Pediatr Surg 14:206–215
Kubler JF, Kos M, Jesch NK et al (2007) Carbon dioxide suppresses macrophage superoxide anion production independent of extracellular pH and mitochondrial activity. J Pediatr Surg 42:244–248
Mogilner JG, Bitterman H, Hayari L et al (2008) Effect of elevated intraabdominal pressure and hyperoxia on portal vein blood flow, hepatocyte proliferation and apoptosis in a rat model. Eur J Pediatr Surg 18:380–386
Tan M, Xu FF, Peng JS et al (2003) Changes in the level of serum liver enzymes after laparoscopic surgery. World J Gastroenterol 9:364–367
Guven HE, Oral S (2007) Liver enzyme alterations after laparoscopic cholecystectomy. J Gastrointestin Liver Dis 16:391–394
Oetzmann von Sochaczewski C, Petersen C et al (2011) Laparoscopic versus conventional Kasai portoenterostomy does not facilitate subsequent liver transplantation in infants with biliary atresia. J Laparoendosc Adv Surg Tech A 22:408–411
Liu SL, Li L, Cheng W et al (2009) Laparoscopic hepatojejunostomy for biliary atresia. J Laparoendosc Adv Surg Tech A 19:S31–S35
Liem NT, Son TN, Quyng TA et al (2010) Early outcomes of laparoscopic surgery for biliary atresia. J Pediatr Surg 45:1665–1667
Yamataka A, Lane GJ, Cazares J (2012) Laparoscopic surgery for biliary atresia and choledochal cyst. Semin Pediatr Surg 21:201–210
Wildhaber BE, Majno P, Mayr J et al (2008) Biliary atresia: Swiss national study, 1994–2004. J Pediatr Gastroenterol Nutr 46:299–307
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wada, M., Nakamura, H., Koga, H. et al. Experience of treating biliary atresia with three types of portoenterostomy at a single institution: extended, modified Kasai, and laparoscopic modified Kasai. Pediatr Surg Int 30, 863–870 (2014). https://doi.org/10.1007/s00383-014-3551-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-014-3551-5