Abstract
Purpose
To determine the clinical characteristics of patients submitted to surgical treatment for non-cystic fibrosis (CF) bronchiectasis, the indications for surgery, and the results obtained at a referral facility for pediatric thoracic surgery.
Methods
Between January 1998 and December 2009, we retrospectively reviewed the medical charts of 109 pediatric patients with non-CF bronchiectasis who underwent surgical treatment. These findings were subsequently analyzed by focusing on postoperative complications and long-term results.
Results
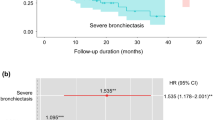
Of the 109 patients undergoing pulmonary resection, the mean age was 7.6 years (ranging from 1 to 15.5 y–o) with male predominance (59 %). The most common procedure was segmentectomy (43 %) followed by left lower lobectomy (38 %). Minor postoperative complications occurred in 36 % of the patients; the most common was transient atelectasis (26 %), followed by air leak (6 %), and postoperative pain (4 %). There was one death within the 30-day postoperative period, but it was unrelated to the procedure. Eighty-three children were followed after discharge, with a mean follow-up period of 667 days. Sixty-five (76 %) patients showed improvement of clinical symptoms after surgery.
Conclusions
Lung resection for the treatment of non-CF bronchiectasis in children is a safe procedure, with no life-treating morbidity and low mortality. This procedure also leads to significant improvements in symptoms and quality of life.


Similar content being viewed by others
References
Byington CL, Spencer LY, Johnson TA, Pavia AT, Allen D, Mason EO, Kaplan S, Carroll KC, Daly JA, Christenson JC, Samore MH (2002) An epidemiological investigation of a sustained high rate of pediatric parapneumonic empyema: risk factors and microbiological associations. Clin Infect Dis 34(4):434–440. doi:CID01092010.1086/338460
Rees JH, Spencer DA, Parikh D, Weller P (1997) Increase in incidence of childhood empyema in West Midlands. Lancet 349(9049):402. doi:S0140673697800220
Barker AF (2002) Bronchiectasis. N Engl J Med 346(18):1383–1393. doi:10.1056/NEJMra012519346/18/1383
Santamaria F, Montella S, Camera L, Palumbo C, Greco L, Boner AL (2006) Lung structure abnormalities, but normal lung function in pediatric bronchiectasis. Chest 130(2):480–486. doi:130/2/48010.1378/chest.130.2.480
Voter KZ, Ren CL (2008) Diagnosis of cystic fibrosis. Clin Rev Allergy Immunol 35(3):100–106. doi:10.1007/s12016-008-8078-x
Fischer GB, Sarria EE, Mattiello R, Mocelin HT, Castro-Rodriguez JA (2010) Post infectious bronchiolitis obliterans in children. Paediatr Respir Rev 11(4):233–239. doi:S1526-0542(10)00064-310.1016/j.prrv.2010.07.005
Bilton D (2008) Update on non-cystic fibrosis bronchiectasis. Curr Opin Pulm Med 14(6):595–599. doi:10.1097/MCP.0b013e328312ed8c00063198-200811000-00015
Karakoc GB, Yilmaz M, Altintas DU, Kendirli SG (2001) Bronchiectasis: still a problem. Pediatr Pulmonol 32(2):175–178. doi:10.1002/ppul.1104
Valery PC, Morris PS, Grimwood K, Torzillo PJ, Byrnes CA, Masters IB, Bauert PA, McCallum GB, Mobberly C, Chang AB (2012) Azithromycin for Indigenous children with bronchiectasis: study protocol for a multi-centre randomized controlled trial. BMC Pediatr 12:122. doi:1471-2431-12-12210.1186/1471-2431-12-122
Marostica PJ, Fischer GB (2006) Non-cystic-fibrosis bronchiectasis: a perspective from South America. Paediatr Respir Rev 7(4):275–280. doi:S1526-0542(06)00032-710.1016/j.prrv.2006.04.008
Haciibrahimoglu G, Fazlioglu M, Olcmen A, Gurses A, Bedirhan MA (2004) Surgical management of childhood bronchiectasis due to infectious disease. J Thorac Cardiovasc Surg 127(5):1361–1365. doi:10.1016/j.jtcvs.2003.11.018S0022522303019834
Steinfort DP, Brady S, Weisinger HS, Einsiedel L (2008) Bronchiectasis in central Australia: a young face to an old disease. Respir Med 102(4):574–578. doi:S0954-6111(07)00452-010.1016/j.rmed.2007.11.007
Sirmali M, Karasu S, Turut H, Gezer S, Kaya S, Tastepe I, Karaoglanoglu N (2007) Surgical management of bronchiectasis in childhood. Eur J Cardiothorac Surg 31(1):120–123. doi:S1010-7940(06)00975-410.1016/j.ejcts.2006.10.021
Kaminski PN, Forgiarini LAJ, Andrade CF (2013) Early respiratory therapy reduces postoperative atelectasis in children undergoing lung resection. Respir Care 58(5):805–809. doi:rc01870r3kaminski10.4187/respcare.01870
Kapur N, Karadag B (2011) Differences and similarities in non-cystic fibrosis bronchiectasis between developing and affluent countries. Paediatr Respir Rev 12(2):91–96
Spencer DA (2005) From hemp seed and porcupine quill to HRCT: advances in the diagnosis and epidemiology of bronchiectasis. Arch Dis Child 90(7):712–714. doi:90/7/71210.1136/adc.2004.054031
Nikolaizik WH, Warner JO (1994) Aetiology of chronic suppurative lung disease. Arch Dis Child 70(2):141–142
Mattiello R, Mallol J, Fischer GB, Mocelin HT, Rueda B, Sarria EE (2010) Pulmonary function in children and adolescents with postinfectious bronchiolitis obliterans. J Bras Pneumol 36(4):453–459. doi:S1806-37132010000400010
Mattiello R, Sarria EE, Stein R, Fischer GB, Mocelin HT, Barreto SS, Lima JA, Brandenburg D (2008) Functional capacity assessment in children and adolescents with post-infectious bronchiolitis obliterans. J Pediatr (Rio J) 84(4):337–343. doi:10.2223/JPED.1807
Al Subie H, Fitzgerald DA (2012) Non-cystic fibrosis bronchiectasis. J Paediatr Child Health 48(5):382–388. doi:10.1111/j.1440-1754.2010.01871.x
Fall A, Spencer D (2006) Paediatric bronchiectasis in Europe: what now and where next? Paediatr Respir Rev 7(4):268–274. doi:S1526-0542(06)00366-610.1016/j.prrv.2006.05.003
Hochhegger B, Irion K, Bello R, Marchiori E, Moreira J, Porto Nda S, Quinto Dos Reis D (2010) Understanding the classification, physiopathology and the diagnostic radiology of bronchiectasis. Rev Port Pneumol 16(4):627–639
Pasteur MC, Bilton D, Hill AT (2010) British Thoracic Society guideline for non-CF bronchiectasis. Thorax 65(Suppl 1):i1–i58. doi:65/Suppl_1/i110.1136/thx.2010.136119
Chang AB, Grimwood K, Robertson CF, Wilson AC, van Asperen PP, O’Grady KA, Sloots TP, Torzillo PJ, Bailey EJ, McCallum GB, Masters IB, Byrnes CA, Chatfield MD, Buntain HM, Mackay IM, Morris PS (2012) Antibiotics for bronchiectasis exacerbations in children: rationale and study protocol for a randomised placebo-controlled trial. Trials 13:156. doi:1745-6215-13-15610.1186/1745-6215-13-156
Masekela R, Green RJ (2012) The role of macrolides in childhood non-cystic fibrosis-related bronchiectasis. Mediators Inflamm 2012:134605. doi:10.1155/2012/134605
Pizzutto SJ, Grimwood K, Bauert P, Schutz KL, Yerkovich ST, Upham JW, Chang AB (2013) Bronchoscopy contributes to the clinical management of indigenous children newly diagnosed with bronchiectasis. Pediatr Pulmonol 48(1):67–73. doi:10.1002/ppul.22544
Hester KL, Macfarlane JG, Tedd H, Jary H, McAlinden P, Rostron L, Small T, Newton JL, De Soyza A (2012) Fatigue in bronchiectasis. QJM 105(3):235–240. doi:hcr18410.1093/qjmed/hcr184
Ferreira HP, Fischer GB, Felicetti JC, Camargo Jde J, Andrade CF (2010) Surgical treatment of congenital lung malformations in pediatric patients. J Bras Pneumol 36(2):175–180. doi:S1806-37132010000200004
Findik G, Gezer S, Sirmali M, Turut H, Aydogdu K, Tastepe I, Karaoglanoglu N, Kaya S (2008) Thoracotomies in children. Pediatr Surg Int 24(6):721–725. doi:10.1007/s00383-008-2144-6
Schneiter D, Meyer N, Lardinois D, Korom S, Kestenholz P, Weder W (2005) Surgery for non-localized bronchiectasis. Br J Surg 92(7):836–839. doi:10.1002/bjs.4949
Gursoy S, Ozturk AA, Ucvet A, Erbaycu AE (2010) Surgical management of bronchiectasis: the indications and outcomes. Surg Today 40(1):26–30. doi:10.1007/s00595-009-4013-x
Kosar A, Orki A, Kiral H, Demirhan R, Arman B (2010) Pneumonectomy in children for destroyed lung: evaluation of 18 cases. Ann Thorac Surg 89(1):226–231. doi:S0003-4975(09)02023-210.1016/j.athoracsur.2009.10.007
Eren S, Eren MN, Balci AE (2003) Pneumonectomy in children for destroyed lung and the long-term consequences. J Thorac Cardiovasc Surg 126(2):574–581. doi:S0022522303005865
Ötgün I, Karnak İ, Tanyel FC, Şenocak ME, Nebil B (2004) Surgical treatment of bronchiectasis in children. J Pediatr Surg 39(10):1532–1536
Streete BG, Salyer JM (1960) Bronchiectases: an analysis of 240 cases treated by pulmonary resection. J Thorac Cardiovasc Surg 40:383–392
Kutlay H, Cangir AK, Enon S, Sahin E, Akal M, Gungor A, Ozdemir N, Kavukcu S (2002) Surgical treatment in bronchiectasis: analysis of 166 patients. Eur J Cardiothorac Surg 21(4):634–637. doi:S1010794002000532
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Andrade, C.F., Melo, I.A., Holand, A.R.R. et al. Surgical treatment of non-cystic fibrosis bronchiectasis in Brazilian children. Pediatr Surg Int 30, 63–69 (2014). https://doi.org/10.1007/s00383-013-3420-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-013-3420-7