Abstract
Purpose
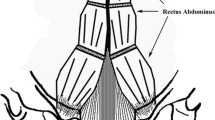
Since 1999, complete primary repair of exstrophy has represented a valid alternative in the treatment of exstrophy patients, offering one- stage reconstruction for all components of this malformation in newborns. The vast majority of cases are currently approached within 48/72 h of life, and risk of vascular injury to penile glans and/or corpora has been reported with increased frequency with this procedure. We report our initial experience with a delayed approach to complete repair, with bladder plate left intact and taken care at home by the parents, while awaiting for the patient to reach adequate weight. Delayed approach also enabled us to preoperatively stimulate phallic size with testosterone, a treatment which was so far confined only to redo or failed cases.
Methods
Six male exstrophy patients were treated over a three-year (2007–2009) period. After initial workup, newborns were discharged home with bladder plate taken care by the parents. A weight of 4,500 g was arbitrarily deemed satisfactory for surgery. While at home, patients underwent preoperative testosterone stimulation (testosterone enanthate, four biweekly administrations of 100 mg/per square meter body surface). In each case biopsies of bladder mucosa were taken at time of surgery. Complications, age at surgery, increases in phallic size were extracted from clinical and surgical case notes.
Results
Weight at surgery ranged from 4,510 to 5,600 g. Age range was 43–91 days. Mean increase in phallic size after testosterone stimulation was 8.3 mm. Three complications were observed: two were suprapubic fistulas, of these, one closed spontaneously and one required surgery subsequently. In one fascial dehiscence emergency closure was needed. Hypospadias occurred in all patients. All histologic specimens demonstrated a mildly inflamed bladder mucosa.
Conclusions
Delayed repair of bladder exstrophy allows to approach patients who have reached adequate weight and stabilization; if adequately cared for bladder plate shows minimal inflammation at surgery and can be managed by the parents at home. Deferring surgery also offers the advantages of preoperative testosterone stimulation, promotion of mother–baby relationship as well as of transfer to Centers with adequate experience and proficiency in all aspects of bladder exstrophy reconstruction.

Similar content being viewed by others
References
Kibar Y, Roth CC, Frimberger D, Kropp BP (2009) Our initial experience with the technique of complete primary repair of exstrophy. J Pediatr Urol 5:186–189
Gearhart J (2001) Complete repair of bladder exstrophy in the newborn: complications and management. J Urol 165:2431–2433
Amukele S, Lee G, Stock J, Hanna M (2003) 20-year experience with iatrogenic penile injury. J Urol 170:1691–1694
Husmann DA, Gearhart JP (2004) Loss of the penile glans and/or corpora following primary repair of bladder exstrophy using the complete penile disassembly technique. J Urol 172:1696–1701
Gargollo PC, Borer J, Diamond DA, Hendren WH, Grant R, Rosoklija I, Retik AB (2008) Prospective followup in patients after complete primary repair of exstrophy. J Urol 180:1665–1670
Hammouda HM, Kote H (2004) Complete primary repair of bladder exstrophy: initial experience wih 33 cases. J Urol 172:1441–1444
Shnorhavorian M, Grady RW, Andersen A, Joyner BD, Mitchell ME (2008) Long term follow up of complete primary repair of exstrophy: the Seattle experience. J Urol 180:1615–1620
Dodson JL, Surer I, Baker LA, Jeffs RD, Gearhart JP (2001) The newborn exstrophy bladder inadequate for primary closure, evaluation, management and outcome. J Urol 165:1656–1659
El-Sherbiny MT, Hafez TA, Ghoneim MA (2002) Complete primary repair of exstrophy: further experience with neonates and children after failed initial closure. A single center experience. J Urol 168:1692–1694
Baskin LS, Sutherland RS, DiSandro MJ, Hayward SW, Lipschutz J, Cunha GR (1997) The effect of testosterone on androgen receptors and human penile growth. J Urol 158:1113–1118
Gearhart JP, Baird AD (2005) The failed complete repair of exstrophy: insights and outcomes. J Urol 174:1669–1673
Grady RW, Mitchell ME (2000) Complete primary repair of exstrophy: surgical technique. Urol Clin N Am 27:569–578
Lais A, Paolocci N, Ferro F (1996) Morphometric analysis of smooth muscle in the exstrophy–epispadias complex. J Urol 156:819–821
Peppas DS, Tchetgen MB, Lee BR (1999) A quantitative histological analysis of the bladder in classical bladder exstrophy in various stages of reconstruction utilizing color morphometry. In: Gearhart JP, Mathews R (eds) The exstrophy–epispadias complex: research concepts and clinical applications. Kluwer Academic/Plenum Publisher, New York, pp 41–47
Mathews R, Gosling JA, Gearhart JP (2004) Ultrastructure of the bladder in classic exstrophy: correlation with development of continence. J Urol 172:1446–1449
Orsola A, Estrada CR, Nguyen HT, Retik AB, Freeman MR, Peters CA, Adam RM (2004) Growth and stretch response of human exstrophy bladder smooth muscle cells: molecular evidence of normal intrinsic function. BJU Int 95:144–148
Olguner M, Akgür FM, Ozdemir T, Aktuğ T, Ozer E (2000) Amniotic fluid exchange for the prevention of neural tissue damage in myelomeningocele: an alternative minimally invasive method to open in utero surgery. Pediatr Neurosurg 33:252–254
Grady RW, Mitchell ME (1999) Complete primary repair of exstrophy. J Urol 162:1415–1420
Wiersma R (2008) Overview of bladder exstrophy: a third world perspective. J Pediatr Surg 43:1520–1523
Borer J, Gargollo PC, Hendren WH, Diamond DA, Peters CA, Atala A, Grant R, Retik AB (2005) Early outcome following complete primary repair of bladder exstrophy in the newborn. J Urol 174:1674–1679
Mitchell ME, Bagli DJ (1998) Newborn exstrophy closure, epispadias repair. World J Urol 16:200–204
Mazer P, Gischler SJ, Koot HM, Tibboel D, van Dijk M, Duivenvoorden HJ (2008) Impact of a child with congenital anomalies on parents (ICCAP) questionnaire; a psychometric analysis. Health Qual Life Outcomes 23:102–106
Nelson CP, Dunn RL, Bloom DA, Wei JT (2005) Contemporary practice patterns in management of bladder exstrophy in newborns. J Urol Suppl 173:1, abstract 2
Gearhart JP, Jeffs R (1985) The use of topical vasodilators in infant renal surgery. J Urol 134:298–300
Woodhouse CJ, Kellet M (1984) Anatomy of the penis and its deformity in exstrophy–epispadias complex. J Urol 132:1122–1124
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zaccara, A., De Gennaro, M., Di Lazzaro, A. et al. Delayed complete repair of exstrophy with testosterone treatment: an alternative to avoid glans complications?. Pediatr Surg Int 27, 417–421 (2011). https://doi.org/10.1007/s00383-010-2745-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-010-2745-8