Abstract
Purpose
We aimed to study the changes in cytokines, oxidative mediators, and pulmonary blood pressure in a neonatal sepsis model when applying an extracorporeal circuit (ECC).
Methods
Of 28 anesthetized and mechanically ventilated 3-day-old piglets, 14 underwent cecal ligation and perforation (CLP), of which 7 underwent ECC for 3 h from 3 to 6 h after CLP. The remaining 14 were sham, of which 7 underwent ECC. Serum interleukin (IL)-6, IL-10, tumor necrosis factor (TNF), interferon gamma (IFN-γ), total hydroperoxide (TH), nitric oxide metabolites (NOx), and mean pulmonary arterial blood pressure (mPAP)/mean arterial blood pressure (mABP) ratio were measured at pre-CLP and at 3, 6, and 9 h in the CLP groups, and continued in the sham groups at 12, 15, 18, and 24 h.
Results
The CLP group with ECCs compared to the CLP group without it showed higher levels of serum IL-6, IL-10, and NOx at 6 h and higher levels of serum TH at 6 and 9 h. The sham group with ECCs compared to the one without it showed higher levels of serum IL-6 and IL-10 at 12, 15, and 18 h, TH at 6 and 9 h, TNF at 6 h, and IFN-γ at 9 h. The mPAP/mABP ratios in the CLP group with ECCs were higher compared to the CLP group without it at 6 and 9 h.
Conclusion
Applying ECCs provoked a window of cytokines, free radicals elevation, and pulmonary hypertension which could be hazardous in critically ill newborns.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The use of extracorporeal circuits (ECCs) in critically ill patients is frequent in adult and neonatal intensive care units for direct hemofiltration, direct hemoperfusion, and extracorporeal membrane oxygenation (ECMO). The contact between the blood and the various artificial surfaces of the extracorporeal system leads to the so-called postperfusion syndrome (or postpump syndrome), which can escalate in severe cases into the systemic inflammatory response syndrome (SIRS) [1], acute lung failure (adults respiratory distress syndrome, ARDS) [2], and sepsis, or even multiple organ failure (MOF) [3].
It has been reported in an in vivo study in adult patients, and in an in vitro study using adult human blood, that applying ECCs would induce some degree of imbalance between oxidants and antioxidants resulting in oxidative stress [4, 5]. On the other hand, in non-septic pediatric patients undergoing cardiopulmonary bypass, ECC application was shown to decrease circulating oxidants with a latent increase in inflammatory mediators [6].
During Gram-negative bacterial sepsis syndrome, the stimulation of macrophages and monocytes by the endotoxin results in the acute release of early inflammatory mediators such as tumor necrosis factor (TNF) and interleukin (IL)-1, and later interferon (IFN)-γ [7].
IL-6, which has been regarded as a proinflammatory cytokine is now considered to be both proinflammatory and anti-inflammatory [8]. On the other hand, IL-10, a well known anti-inflammatory cytokine, plays an important role in the development of a syndrome known as compensatory anti-inflammatory response syndrome (CARS) [9]. Furthermore, it has been reported that reactive oxygen species (ROS) and nitric oxide (NO) play a significant role in the pathogenesis of neonatal sepsis and its complications [10]. The total hydroperoxide (TH) represents a measure of overall oxidative damage; it includes the intermediate oxidative of lipids, peptide, and amino acids [11].
The immunological response to infection in neonates differs compared to elder children and adults [12], and therefore the neonatal immune response when exposed to an immunological stimulant may be different or manifest in another manner than what is observed in elder children or in adults.
In neonatal sepsis, the hemodynamic features differ from adult sepsis exhibiting more severe circulatory impairment. The time course of septic hemodynamic responses typically consists of two phases: a hyperdynamic phase and a hypodynamic phase. The hyperdynamic phase is characterized by an early decrease in systemic resistance and increase in cardiac output and heart rate, and the hypodynamic phase is characterized by a decrease in mean arterial blood pressure accompanied by a significant fall in cardiac output [13]. The hemodynamic states are highly influenced by myocardial function, including both diastolic and systolic states, as well as systemic and pulmonary vascular resistance during the different phases of neonatal sepsis and septic shock.
This study was to evaluate the changes in the immunological response and the pulmonary blood pressure after applying an ECC to a characterized neonatal sepsis model cecal ligation and perforation (CLP) and its sham [14].
Materials and methods
Animal preparation
The experiments were performed in adherence to National Institute of Health guidelines on the use of experimental animals, and the protocol was approved by the Animal care and Use and the Ethics Committee of the Nagoya City University Graduate School of Medical Sciences. Twenty-eight (7 in each of four groups: CLP with ECCs, CLP without ECCs, sham with ECCs, and sham without ECCs) mixed-strain newborn piglets were obtained on their third day of life from a local farmer. They were transported on the day of the procedure. The mean body weight was 1,690 ± 62.7 g (mean ± SEM) in the CLP group with ECCs, 1,760 ± 35.6 g in the CLP group without ECCs, 1,775 ± 184 g in the sham group with ECCs, and 1,715 ± 91.4 g in the sham group without ECCs. The piglets were premedicated with ketamine chloride (10 mg/kg intramuscularly), after which anesthesia was induced with pentobarbital sodium (20 mg/kg intravenously) and maintained by a continuous infusion of pentobarbital sodium (5 mg/kg/h) in 5% glucose solution via a peripheral line at a rate of 5 ml/kg/h throughout the study to avoid hypovolemia. All surgical procedures were performed under sterile conditions. Each piglet underwent a tracheotomy and was intubated with an endotracheal tube (internal diameter 4.0 mm) and ventilated with an infant ventilator (model IV-100, Sechrist, Anaheim, CA, USA). The inspiration/expiration pressures were initially set at 14/4 cm H2O with an inspiration time of 0.5 s under room air. A cut-down procedure was used to insert a 3-Fr polyvinyl catheter in the left femoral artery for measuring the mean systemic blood pressure (mABP) and for withdrawing blood samples. A 4-Fr Berman angiographic catheter (American Edwards Laboratories, Irvine, CA, USA) was inserted under fluoroscopy via the right external jugular vein and placed in the main pulmonary artery to measure the mPAP. The mABP and mPAP were measured with a neonatal monitor (model 78801 B, Hewlett Packard, Andover, MA, USA), and the data were collected with a MacLab/8s system (ADI Instruments, Mountain View, CA, USA). Relative pulmonary hypertension was evaluated using the ratio mPAP/mABP. To prevent hypothermia, body temperature was maintained using a thermal pad and a polyvinyl cover and was monitored by a rectal probe.
Body temperature was maintained by a thermal pad and monitored by a rectal probe. Modified cecal ligation and perforation (cecal devascularization and perforation) was performed on the two CLP groups as previously explained [14]. This sepsis model was reported to be bacteremic with Gram-negative enteric organisms, and some contained anaerobic organisms [14]. Also the model was previously reported to show significant high levels of endotoxin after 6 h from CLP [14, 15].
Animals in the sham groups underwent the paramedian incision and not the CLP procedure.
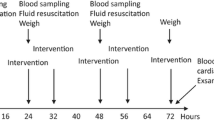
The ECCs application
The ECCs were formed of polyvinylchloride (AP chamber set 15 m, Niporo Corp, Tokyo, Japan) and a peristaltic pump (Iwaki PST-110, Asahi Techno Glass Corp, Tokyo, Japan) between the right femoral artery and the left external jugular vein (arteriovenous ECCs). The ECCs were filled with 20 cc of blood from a donor piglet. Cross matching was done before the CLP procedure. Blood flow rate through this circuit was 3 ml/kg/min. The ECCs application started after the 3 h sampling for 3 h until the 6 h sampling time. Low-molecular-weight heparin was applied as an anticoagulant just before the ECCs were started.
Survival and experimental protocol
The study was continued until the time of spontaneous death in the two CLP groups and continued in the two sham groups until 24 h when they were killed with a lethal dose of pentobarbital sodium. The survival time in the CLP with ECCs was shorter than in the CLP without ECCs (9.4 ± 0.4 vs. 11.6 ± 1 h, p < 0.05), and both were shorter than in the two sham groups.
In each group, blood samples for IL-6, IL-10, TNF, IFN-γ, NOx, and TH assays were aseptically collected from the femoral arterial catheter. Blood samples were taken pre-CLP and at 3, 6, and 9 h after CLP in the two CLP groups and were continued in the sham groups at 12, 15, 18, and 24 h. Each sample was placed into pyrogen-free sterilized tubes.
Measurements
Serum IL-6, IL-10, and TNF were measured using an immunoassay kit specific for porcine IL-6, IL-10, and TNF, respectively (GT, Minneapolis, MN, USA). Serum IFN-γ was measured using ELISA kit specific for porcine IFN-γ (BioSource International, Camarillo, CA, USA). Duplicate measurements were performed for each sample. The concentrations were calculated based on the obtained standard curves. Nitric oxide metabolites were evaluated by measurement of serum concentration of NO2 − + NO3 − (NOx). NOx concentration was measured using PFA-310 NO (F.I.A instruments Co., Tokyo, Japan).
The TH production was measured with the free radical analytic system (FRAS), using the reactive oxygen metabolites (d-ROMs) kit (Diacron srl, Italy), as previously described [16].
Statistical analysis
The distributions of data were tested using the Shapiro–Wilk test. The mean of the four groups (inter-groups) at the same time point until 9 h were compared using the analysis of variance (ANOVA) for repeated measures, followed by the Tukey–Kramer post hoc test. After 9 h, the Mann–Whitney test was used to compare between the two sham groups. Data are reported as mean ± SEM. Probability values of less than 0.05 were considered significant. Differences in survival between the two groups were calculated using the Kaplan–Meier test and were compared using the Kruskal–Wallis test followed by the Mann–Whitney test. All data analyses were performed with commercially available statistical analysis software package SPSS (Statistical Package for Social Sciences, Chicago, IL, USA).
Results
There were no differences between the four groups in their cytokines, NOx, or TH levels at pre-CLP. There were none between the two CLP groups or between the two sham groups in their serum levels of cytokines, NOx, or TH until 6 h samples were taken.
Effects on IL-6 and IL-10
After the ECCs were applied, the serum IL-6 and IL-10 levels became higher in the CLP group with ECCs than in the CLP group without them at 6 h (Fig. 1a, b). The mean IL-6 and IL-10 serum levels remained higher at 9 h in the CLP group with ECCs, but these differences did not reach significance (Fig. 1a, b).
Serial serum measurements of a IL-6 and b IL-10 in CLP neonatal sepsis model (n = 7), CLP with ECCs (n = 7), sham (n = 7), and sham with ECCs (n = 7) until 9 h. The measurements continued in the two sham groups until 24 h. *3 h is the time of starting the extracorporeal circuit; **6 h is the time of stopping the extracorporeal circuit. †The difference between the CLP groups († p < 0.05). ‡The difference between the CLP and sham groups without ECCs (‡ p < 0.05). The difference between the CLP and sham groups with ECCs (p < 0.05). ※The difference between the sham groups (※ p < 0.05)
IL-6 serum levels in both CLP groups became higher than in both sham groups at 3, 6, and 9 h. In the sham group with ECCs, IL-6 became higher than in the sham group without ECCs at 12, 15, and 18 h. At 24 h, serum IL-6 in the sham group with ECCs returned to near the levels in the sham group without them (Fig. 1a).
Serum IL-10 levels in the sham group with ECCs became higher than in the sham group without them at 6, 12, 15, 18, and 24 h (Fig. 1b).
Effects on TNF and IFN-γ
Serum levels of TNF and IFN-γ showed no differences between the two CLP groups, one with and one without ECCs, throughout the study.
The TNF serum levels in both CLP groups were higher than in both sham groups with and without ECC at 3, 6, and 9 h. The mean TNF serum levels in the sham group with ECCs were higher than in the other sham group at 6 h and maintained higher levels until the 24 h samples, but a significant difference was detected between the two shams only at 6 h (Fig. 2a).
Serial serum measurements of a TNF and b IFN-γ in CLP neonatal sepsis model (n = 7), CLP with ECCs (n = 7), sham (n = 7), and sham with ECCs (n = 7) until 9 h. The measurements continued in the two sham groups until 24 h. *3 h is the time of starting the extracorporeal circuit; **6 h is the time of stopping the extracorporeal circuit. ‡The difference between the CLP and sham groups without ECCs (‡ p < 0.05). The difference between both the CLP and sham groups with ECCs (p < 0.05). ※The difference between the sham groups (※ p < 0.05)
The serum levels of IFN-γ showed no differences among all four groups until 9 h when serum IFN-γ levels were higher in both CLP groups than in both sham groups with and without ECCs. Later, at 12 h, the IFN-γ serum levels in the sham group with ECCs were higher than in the other sham group (Fig. 2b).
Effects on serum NOx and TH
At 3 h, the serum levels of NOx were higher in both CLP groups with and without ECCs compared to both sham groups. At 6 h, the serum levels of NOx were higher in the CLP group with ECCs than in the group without it. The NOx serum levels in the CLP group with ECCs were higher than in both sham groups at 6 h.
The mean NOx serum levels in the CLP group without ECCs were higher than in both sham groups at 6 h, but these differences were significant only compared to the levels in the sham group without ECCs. No differences were found between the two sham groups in their NOx serum levels throughout the study (Fig. 3a).
Serial serum measurements of a NOx and b TH in CLP neonatal sepsis model (n = 7), CLP with ECCs (n = 7), sham (n = 7), and sham with ECCs (n = 7) until 9 h. The measurements continued in the two sham groups until 24 h. *3 h is the time of starting the extracorporeal circuit; **6 h is time of stopping the extracorporeal circuit. †The difference between the CLP groups († p < 0.05). ‡The difference between the CLP and sham groups without ECCs (‡ p < 0.05). The difference between both the CLP and sham groups with ECCs (p < 0.05). ※The difference between the sham groups (※ p < 0.05). One Carr unit corresponds to the color development caused by a H2O2 solution at a concentration of 0.08%
Serum TH became higher in the CLP group with ECCs than in both CLP groups at 6 and 9 h. The mean TH serum levels in the sham group with ECCs became higher than in both the CLP groups at 6 and 9 h, but the differences did not reach significance. This difference was maintained between the two sham groups with and without ECCs at 12, 15, 18, and 24 h. (Fig. 3b).
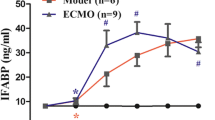
Effect on pulmonary blood pressure
The mPAP/mABP ratios in the CLP group with ECCs were higher compared to the CLP group without it at 6 and 9 h (0.96 ± 0.132 vs. 0.79 ± 0.05 and 1.07 ± 0.15 vs. 0.85 ± 0.12, p < 0.05 and 0.05), respectively (Fig. 4).
Serial measurement of mPAP/mABP in CLP neonatal sepsis model (n = 7) (closed triangle and continuous line), CLP with ECCs (n = 7) (open triangle and interrupted line), sham (n = 7) (closed square and continuous line), and sham with ECCs (n = 7) (open square and interrupted line) until 9 h. The measurements continued in the two sham groups until 24 h. *3 h is the time of starting the extracorporeal circuit; **6 h is the time of stopping the extracorporeal circuit. †The difference between the CLP groups († p < 0.05). ‡The difference between the CLP and sham groups without ECCs (‡ p < 0.05). The difference between the CLP and sham groups with ECCs (p < 0.05). The error bar represents the SEM
Discussion
In our study on a neonatal sepsis model, the CLP caused the proinflammatory mediators (TNF and IL-6) to take the upper hand before we applied the ECC, but similar changes were not evident in serum levels of the anti-inflammatory cytokine IL-10. This immunological balance was due to the active response against the systemic infection induced by the CLP procedure, but after exposure to the ECCs, both the proinflammatory and the anti-inflammatory serum levels were elevated. Toft et al. detected that applying an extracorporeal circuit in a continuous venovenous hemofiltration did not increase the serum levels of the proinflammatory mediator IL-8 or the anti-inflammatory mediator IL-10 in a healthy porcine model [17], and not a critically ill newborn as in the present study. The main source of IL-6 and IL-10 production in human and murine models are CD4 Th2 cells, CD8 T cells, and monocytes/macrophages [18]. The CD4 cell clones can be classified into two populations on the basis of cytokine production, Th1 and Th2, with different cytokine pattern and immune functions [19]. Th1 lymphocytes produce proinflammatory cytokines such as TNF [20].
On the other hand, Th2 lymphocytes produce mainly IL-4, IL-6, IL-10, and IL-13 [21]. In our study an application of ECCs was associated with Th2 polarization, which was evident by the overproduction of IL-6 and IL-10.
The natural killer (NK) cells, which are important producers of IFN-γ, are known to be immature in neonates, and though changes in the NK cell count and activity were not directly evaluated in this study, IFN-γ changes may reflect the changes in NK cell count and activity [12].
It has been hypothesized that during the pathophysiology of sepsis, endotoxin and/or proinflammatory cytokines induce the overproduction of nitric oxide (NO), via inducible NO synthase [5]. NO metabolites (NOx), nitrite and nitrate, have been used as indicators of NO production and have shown an elevation of serum NOx concentration in adult patients suffering from sepsis [22] and in neonatal sepsis [23]. McDonagh et al. [4], using adult blood in an in vitro study, showed that ECC increased the production of ROS. Our study showed similar results, but in an in vivo study, where NOx serum levels were higher in the CLP group with ECCs, and TH was also higher in both the CLP group and the sham group after the ECC applications.
Our overall results show that the ECC caused the Th2 cytokines and free radicals to be markedly elevated when applied to the CLP model more than the changes in these mediators caused by CLP only.
Another study reported on the role of nitric oxide and cyclooxygenase products in pulmonary hypertension during septic shock [24]. During septic shock, these mediators play roles in circulatory impairment by inducing systemic hypotension and pulmonary hypertension. The circulatory changes complicating neonatal sepsis are associated with elevated levels of cytokines and inflammatory mediators such as TNF-α, IL-1β, nitric oxide, and free radicals [25].
Pulmonary vascular tone during the neonatal period shows a lot of instability [26]. This natural instability, along with the effect of the cytokine storm that occurs during sepsis, severely impairs pulmonary vascular tone and pulmonary blood flow with elevation of pulmonary blood pressure causing pulmonary hypertension [24]. This is associated with severe left ventricular dysfunction during neonatal septic shock [26].
TNF-α, IL-1β, and over-abundant NO directly induce myocardial depression during sepsis [27]. TNF-α administered to human and animal myocardial tissue in vitro yields a concentration-dependent depression of contractility [28]. Moreover, removal of TNF-α from the serum or administration of an anti-TNF-α monoclonal antibody reverses this myocardial depressant effect [28]. The higher levels of inflammatory cytokines (TNF-α and IL-6) and free radicals (TH and NO) in the CLP group with ECCs compared to the CLP group without them could explain why the former are exhibiting more levels of pulmonary hypertension. However, other factors caused by the ECC application could have participated in the marked elevation of inflammatory mediators, free radicals, and pulmonary blood pressure in the CLP with ECC compared to the CLP group only.
The changes in the inflammatory mediators together with the increase in free radicals and severer pulmonary hypertension resulting from ECC exposure may have resulted in a slightly shorter survival time in the CLP group with ECCs compared to the CLP group without them.
The application of an extracorporeal circuit provoked a window period of elevated serum cytokines and oxidative mediators in a neonatal sepsis model and its sham, which could be hazardous and should be considered during the treatment of critically ill newborns exposed to extracorporeal circuits.
References
Taylor KM (1996) SIRS—the systemic inflammatory response syndrome after cardiac operations. Ann Thorac Surg 61(6):1607–1608. doi:0003-4975(96)00225-1[pii]
Nieman G, Searles B, Carney D, McCann U, Schiller H, Lutz C, Finck C, Gatto LA, Hodell M, Picone A (1999) Systemic inflammation induced by cardiopulmonary bypass: a review of pathogenesis and treatment. J Extra Corpor Technol 31(4):202–210
Cooper JR Jr, Abrams J, Frazier OH, Radovancevic R, Radovancevic B, Bracey AW, Kindo MJ, Gregoric ID (2006) Fatal pulmonary microthrombi during surgical therapy for end-stage heart failure: possible association with antifibrinolytic therapy. J Thorac Cardiovasc Surg 131(5):963–968. doi:S0022-5223(06)00085-7[pii]
McDonagh P, Cerney K, Hokama J, Lai G, Gonzales R, Davis-Gorman G, Copeland J (2001) Perflubron emulsion reduces inflammation during extracorporeal circulation. J Surg Res 99(1):7–16. doi:10.1006/jsre.2001.6141
Kilbourn RG, Griffith OW (1992) Overproduction of nitric oxide in cytokine-mediated and septic shock. J Natl Cancer Inst 84(11):827–831
Christen S, Finckh B, Lykkesfeldt J, Gessler P, Frese-Schaper M, Nielsen P, Schmid ER, Schmitt B (2005) Oxidative stress precedes peak systemic inflammatory response in pediatric patients undergoing cardiopulmonary bypass operation. Free Radic Biol Med 38(10):1323–1332. doi:S0891-5849(05)00034-1[pii]
Hesse DG, Tracey KJ, Fong Y, Manogue KR, Palladino MA Jr, Cerami A, Shires GT, Lowry SF (1988) Cytokine appearance in human endotoxemia and primate bacteremia. Surg Gynecol Obstet 166(2):147–153
Opal SM, DePalo VA (2000) Anti-inflammatory cytokines. Chest 117(4):1162–1172
Bone RC (1996) Sir Isaac Newton, sepsis, SIRS, and CARS. Crit Care Med 24(7):1125–1128
Batra S, Kumar R, Seema, Kapoor AK, Ray G (2000) Alterations in antioxidant status during neonatal sepsis. Ann Trop Paediatr 20(1):27–33
Buonocore G, Perrone S, Longini M, Terzuoli L, Bracci R (2000) Total hydroperoxide and advanced oxidation protein products in preterm hypoxic babies. Pediatr Res 47(2):221–224
Zaghouani H, Hoeman CM, Adkins B (2009) Neonatal immunity: faulty T-helpers and the shortcomings of dendritic cells. Trends Immunol 30(12):585–591. doi:S1471-4906(09)00172-0[pii]
Yang S, Cioffi WG, Bland KI, Chaudry IH, Wang P (1999) Differential alterations in systemic and regional oxygen delivery and consumption during the early and late stages of sepsis. J Trauma 47(4):706–712
Kato T, Hussein MH, Sugiura T, Suzuki S, Fukuda S, Tanaka T, Kato I, Togari H (2004) Development and characterization of a novel porcine model of neonatal sepsis. Shock 21(4):329–335. doi:00024382-200404000-00007[pii]
Hussein MH, Kato T, Sugiura T, Daoud GA, Suzuki S, Fukuda S, Sobajima H, Kato I, Togari H (2005) Effect of hemoperfusion using polymyxin B-immobilized fiber on IL-6, HMGB-1, and IFN gamma in a neonatal sepsis model. Pediatr Res 58(2):309–314. doi:01.PDR.0000169995.25333.F7[pii]
Dohi K, Satoh K, Ohtaki H, Shioda S, Miyake Y, Shindo M, Aruga T (2005) Elevated plasma levels of bilirubin in patients with neurotrauma reflect its pathophysiological role in free radical scavenging. In Vivo 19(5):855–860
Toft P, Brix-Christensen V, Baech J, Krog J, Jorgensen HS, Tonnesen E, Petersen TK, Dagnaes-Hansen F (2002) Effect of hemodiafiltration and sepsis on chemotaxis of granulocytes and the release of IL-8 and IL-10. Acta Anaesthesiol Scand 46(2):138–144. doi:aas460203[pii]
Lyons A, Kelly JL, Rodrick ML, Mannick JA, Lederer JA (1997) Major injury induces increased production of interleukin-10 by cells of the immune system with a negative impact on resistance to infection. Ann Surg 226(4):450–458 discussion 458–460
Abbas AK, Murphy KM, Sher A (1996) Functional diversity of helper T lymphocytes. Nature 383(6603):787–793. doi:10.1038/383787a0
Nagarkatti M, Clary SR, Nagarkatti PS (1990) Characterization of tumor-infiltrating CD4+ T cells as Th1 cells based on lymphokine secretion and functional properties. J Immunol 144(12):4898–4905
Spellberg B, Edwards JE Jr (2001) Type 1/type 2 immunity in infectious diseases. Clin Infect Dis 32(1):76–102. doi:CID000484[pii]
Ochoa JB, Udekwu AO, Billiar TR, Curran RD, Cerra FB, Simmons RL, Peitzman AB (1991) Nitrogen oxide levels in patients after trauma and during sepsis. Ann Surg 214(5):621–626
Figueras-Aloy J, Gomez L, Rodriguez-Miguelez JM, Jordan Y, Salvia MD, Jimenez W, Carbonell-Estrany X (2003) Plasma nitrite/nitrate and endothelin-1 concentrations in neonatal sepsis. Acta Paediatr 92(5):582–587
Yamamoto S, Burman HP, O’Donnell CP, Cahill PA, Robotham JL (1997) Endothelin causes portal and pulmonary hypertension in porcine endotoxemic shock. Am J Physiol 272(3 pt 2):H1239–H1249
Silveira RC, Procianoy RS (1999) Evaluation of interleukin-6, tumour necrosis factor-alpha and interleukin-1beta for early diagnosis of neonatal sepsis. Acta Paediatr 88(6):647–650
Pollack MM, Fields AI, Ruttimann UE (1984) Sequential cardiopulmonary variables of infants and children in septic shock. Crit Care Med 12(7):554–559
Haworth SG (2006) Pulmonary endothelium in the perinatal period. Pharmacol Rep 58(Suppl):153–164
Kumar A, Thota V, Dee L, Olson J, Uretz E, Parrillo JE (1996) Tumor necrosis factor alpha and interleukin 1beta are responsible for in vitro myocardial cell depression induced by human septic shock serum. J Exp Med 183(3):949–958
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hussein, M.H., Daoud, G.AH. & Hashimoto, T. Elevated inflammatory mediators and pulmonary hypertension after applying an extracorporeal circuit in a neonatal sepsis model. Pediatr Surg Int 27, 53–60 (2011). https://doi.org/10.1007/s00383-010-2727-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-010-2727-x