Abstract
Introduction
Anorectal malformations represent a continuing challenge for the paediatric surgeon. Faecal and urinary incontinence can occur even with an excellent anatomic repair. We undertook a prospective evaluation of comorbidity and psychosocial needs in children and adolescents with anorectal malformation to test the hypothesis whether psychosocial workup in concert with an improved continence situation would lead to a better functional outcome in patients suffering from defecating disorders. Treatment of defecating disorder was based on differentiation between overflow pseudo-incontinence and true faecal incontinence.
Materials and methods
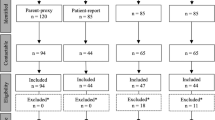
Patients who presented with soiling regardless of the type of anomaly were included in the study: 44 patients were investigated, 14 patients did not meet the criteria of the study, 30 patients aged 4–18 were evaluated. The surgical diagnostic program comprised a careful clinical history, physical examination, exact classification of the malformation, evaluation for associated defects, stool protocol.
Results
Patients were grouped in two different management programs according to their continence situation. Patients with pseudo-incontinence were treated with enemas, diet, anal hygiene, behavioural therapy and physiotherapy. Patients with true faecal incontinence were included in a bowel management program: 28 patients were free of symptoms of soiling after 3 days of hospital treatment and remained free of symptoms 6 months and 1 year later at re-evaluation. Two patients did not follow the therapeutic regime and therefore did not show an improved condition concerning soiling in the long run.
Conclusion
Differentiating between overflow pseudo-incontinence and true faecal incontinence is the basis of an effective treatment of defecating disorders. All patients born with anorectal malformation can be kept clean of stool if they are subjected to an adequate treatment. A multidisciplinary approach is a valuable supplement to standard therapy.
Similar content being viewed by others
References
Pena A (1995) Anorectal malformations. Semin Pediatr Surg 4(1):35–47
Holschneider A, Hutson J, Pena A, Bekhit E, Georgeson K, Iwai N et al (2005) Preliminary report on the international conference for the development of standards for the treatment of anorectal malformations. J Pediatr Surg 40:1521–1526
Kasper H (1985) Ernährungsmedizin und Diätetik. Urban and Schwarzenberg, Munich
Pena A, Guardino K, Tovilla JM et al (1998) Bowel management for fecal incontinence in patients with anorectal malformations. J Pediatr Surg 33:133–137
Koltai JL, Pistor G (1985) Anorektale Inkontinenz. Urban and Schwarzenberg, Munich
Levitt M, Pena A (2005) Outcomes from the correction of anorectal malformations. Curr Opin Pediatr 17(3):394–401
Rintala R, Mildh L, Lindahl H (1992) Fecal continence and quality of life in adult patients with an operated low anorectal malformation. J Pediatr Surg 27(7):902–905
Rintala R, Mildh L, Lindahl H (1994) Fecal continence and quality of life in adult patients with an operated high or intermediate anorectal malformation. J Pediatr Surg 29(6):770–780
Holschneider A (1983) Treatment and functional results of anorectal continence in children with imperforate anus. Acta Chir Belg 82(3):191–204
Holschneider A (1990) Diagnosis and primary surgical therapy of anorectal abnormalities with regard to postoperative incontinence. Zentralbl Chir 115(22):1409–1422
Stelzner F (2001) Anatomie und Entwicklungsgeschichte des anorektalen Kontinenzorgans. Chir Gastroenterol 17:194–201
Holschneider A, Koebke J, Meier-Ruge W, Land N, Jesch NK (2001) Pathophysiology of chronic constipation in anorectal malformations. Eur J Pediatr Surg 11:305–310
Pena A, Levitt MA (2002) Colonic inertia disorders. Curr Probl Surg 39:666–730
van Kuyk EM, Wissink-Essink M, Brugman-Boezeman AT, Oerlemans HM, Nijhuis-van der Sanden MW, Severijnen RS et al (2001) Multidisciplinary behavioral treatment of defecation problems: a controlled study in children with anorectal malformations. J Pediatr Surg 36:1350–1356
van-Kuyk EM, Brugman-Boezeman AT, Wissink-Essink M et al (2000) A biopsychosocial treatment of defecation problems in children with anal atresia: a retrospective study. Pediatr Surg Int 16:317–321
Van-der-Plas RN, Benninga MA, Redekop WK et al (1996) Randomised trial of biofeedback training for encopresis. Arch Dis Child 75:367–374
Cox DJ, Sutphen J, Borowitz S et al (1998) Contribution of behavior therapy and biofeedback to laxative therapy in the treatment of pediatric encopresis. Ann Behav Med 20:70–76
Schmiedecke E, Busch M, Stamatopoulos E, Lorenz C (2008) Multidisciplinary behavioural treatment of fecal incontinence and constipation after correction of anorectal malformation. World J Pediatr 4(3):206–210
Langemeijer RA, Molenaar JC (1991) Continence after posterior sagittal anorectoplasty. J Pediatr Surg 26:587–590
Conflict of interest statement
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Maerzheuser, S., Schmidt, D., Mau, H. et al. Prospective evaluation of comorbidity and psychosocial need in children and adolescents with anorectal malformation. Part one: paediatric surgical evaluation and treatment of defecating disorder. Pediatr Surg Int 25, 889–893 (2009). https://doi.org/10.1007/s00383-009-2440-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-009-2440-9