Abstract
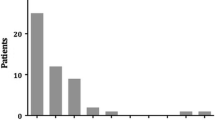
Common pancreaticobiliary channel malunion (PBM) is known to be associated with increased frequency of gallbladder (GB) cancer in adults. Few studies have reported the presence of histological changes in the GB following transduodenal drainage procedures in children with PBM. The aim of this study was to document the histological changes in the GB in children who underwent interval prophylactic cholecystectomy up to 18 years following PBM drainage procedure. All children who underwent open transduodenal sphincterotomy (TDS) for symptomatic PBM followed by prophylactic synchronous (open) and interval (laparoscopic) cholecystectomy between 1987 and 2007 were studied retrospectively. Eight children with PBM were identified. The median age at initial presentation and open transduodenal sphincterotomy was 8 months (1 month–3.5 years). The average interval between open TDS and prophylactic cholecystectomy was 5.5 years (0–18 years). Two children had synchronous TDS and cholecystectomy. At initial presentation, all patients presented with obstructive jaundice. Mild common bile duct dilatation was encountered in all patients. The dilated ducts returned to normal, and remained normal after transduodenal sphincterotomy. Histopathology in seven out of eight GB specimens (87.5%) showed microscopic evidence of chronic inflammation. Chronic cholecystitis (n = 7), Rokitansky–Aschoff sinuses (n = 3), cholesterosis (n = 1) and intestinal metaplasia (n = 1) were observed in the GB biopsies. Only one patient, who had TDS and a synchronous cholecystectomy in the neonatal period, did not have histological changes in the GB. Average follow-up in years ranged between 3 months and 19 years (from TDS) with a median of 8 years, and between 3 months and 6 years (from cholecystectomy) with a median of 2 years. Chronic inflammatory changes were found in seven of eight GB specimens from patients with PBM despite previous drainage procedure in six patients and in one of two patients who underwent synchronous TDS and cholecystectomy. These changes may be the precursor of malignant transformation in GB of patients with PBM.
Similar content being viewed by others
References
Funabiki T, Matsubara T, Ochiai M et al (1997) Surgical strategy for patients with pancreaticobiliary maljunction without choledochal dilatation. Keio J Med 46:169–172
Kimura K, Ohto M, Saisho H, Unozawa T, Tsuchiya Y, Morita M et al (1985) Association of gallbladder carcinoma and anomalous pancreaticobiliary ductal union. Gastroenterology 89:1258–1265
Pushparani P, Redkar RG, Howard ER (2000) Progressive biliary pathology associated with common pancreato-biliary channel. J Pediatr Surg 35:649–651. doi:10.1053/jpsu.2000.0350649
Kusano T, Isa T, Tsukasa K et al (2002) Long-term results after cholecystectomy alone for patients with pancreaticobiliary maljunction without bile duct dilatation. Int Surg 87:107–113
Aoki T, Tsuchida A, Kasuya K et al (2001) Is preventive resection of the extrahepatic bile duct necessary in case of pancreaticobiliary maljunction without dilatation of the bile duct? Jpn J Clin Oncol 31:107–111. doi:10.1093/jjco/hye020
Nagata E, Sakai K, Kinoshita H et al (1985) The relation between carcinoma of the gallbladder and an anomalous connection between the choledochus and the pancreatic duct. Ann Surg 202:182–190. doi:10.1097/00000658-198508000-00008
Miyano T, Ando K, Yamataka A et al (1996) Pancreaticobiliary maljunction associated with nondilatation or minimal dilatation of the common duct in children: diagnosis and treatment. Eur J Pediatr Surg 6:334–337
Barker AP, Ford WDA, LeQuesne GW, Moore DJ (1992) The common bilio-pancreatic channel syndrome in childhood. Aust N Z J Surg 62:70–73. doi:10.1111/j.1445-2197.1992.tb05357.x
Hu B, Gong B, Zhou DY (2003) Association of anomalous pancreatobiliary ductal junction with gallbladder carcinoma in Chinese patients: an ERCP study. Gastrointest Endosc 57:541–545. doi:10.1067/mge.2003.136
Kamisawa T, Okamoto A (2006) Biliopancreatic and pancreatobiliary refluxes in cases with and without pancreaticobiliary maljunction: digestive and clinical implications. Digestion 73:228–236. doi:10.1159/000095424
Stringer M (2002) Choledochal cysts. In: Howard ER, Stringer MD, Colombani PM (eds) Surgery of the liver, bile ducts and pancreas in children, 2nd edn. Arnold Publishers, London
Kinoshita H, Nagata E, Hirohashi K et al (1984) Carcinoma of the gallbladder with an anomalous connection between the choledochus and the pancreatic duct. Report of 10 cases and review of the literature in Japan. Cancer 4:762–769. doi:10.1002/1097-0142(1984)54:4<762::AID-CNCR2820540429>3.0.CO;2-K
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ali, A.E., Blythe, A.I. & Ford, W.D.A. Chronic inflammatory changes seen in gallbladders of patients with pancreatico-biliary malunion years after transduodenal sphincterotomy: is it a precursor for gallbladder carcinoma?. Pediatr Surg Int 24, 1005–1008 (2008). https://doi.org/10.1007/s00383-008-2197-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-008-2197-6