Abstract
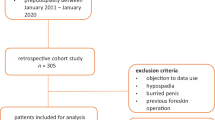
Phimosis has been defined as unretractable foreskin without adherences and/or a circular band of tight prepuce preventing full retraction. The aim of this study is to evaluate the efficacy (response rate) of topical steroids for the treatment of tight phimosis at different age stages. After using the same medication with different dosage schemes, a retrospective analysis was carried out to assess the efficacy of topical steroids in the treatment of tight phimosis. Patients were divided into three groups: group A (betamethasone scheme A), group B (betamethasone scheme B) and group C (control group). Remission of phimosis, with a complete exposure and without a narrowing behind the glans, was considered a complete response to treatment. The outcomes were then related to dosage scheme and patient’s age. The dosage for group A was more effective than the dosage for groups B and C (control group). Phimosis resolved in 90% (group A), 72% (group B) and 56% (group C) of cases. A successful treatment was closely related to the age of patients at the beginning of steroid application. The results showed that treatment with topical steroids, which in general gives good results, proved to be much more successful in patients aged between 4 and 8 years, suggesting the efficacy of an early beginning of the treatment.



Similar content being viewed by others
References
Jorgensen ET, Svenson A (1993) The treatment of phimosis in boys with a potent topical steroid (clobetsol propinate 0.05%) cream. Acta Derm Venerol 3:673–676
Monsour MA, Rabinovitch HH, Dean GE (1999) Medical management of phimosis in children: our experience with topical steroids. J Urol 162:1162–1164
Atilla MK, Dundaroz R, Odabas O, Ozturk H et al (1997) A non surgical approach to the treatment of phimosis: local nonsteroidal anti-inflammatory ointment application. J Urol 158:196–197
Chu CC, Chen KC, Diau GY (1999) Topical steroid treatment of phimosis in boys. J Urol 162:861–863
Iken A, Ben Mouelli S, Fontaine E, Quenneville V et al (2002) Treatment of phimosis with locally applied 0.05% clobetasol propionate. Prospective study with 108 children. Prog Urol 12:1268–1271
Van Basten JP, De Vijlder AM, Mensink HJ (2003) The use of corticosteroid cream to treat phimosis. Ned Tijdschr Geneeskd 147:1544–1547
Elmore JM, Baker LA, Snodgrass WT (2002) Topical steroid therapy as an alternative to circumcision for phimosis in boys younger than 3 years. J Urol 168:1746–1747
Ashfield JE, Nickel KR, Siemens DR, MacNeily AE, Nickel JC (2003) Treatment of phimosis with topical steroids in 194 children. J Urol 169:1106–1108
Orsola A, Caffaratti J, Garat JM (2000) Conservative treatment of phimosis in children using a topical steroid. Urology 56:307–310
Webster TM, Leonard MP (2002) Topical steroid therapy for phimosis. Can J Urol 9:1492–1495
Kikiros CS, Beasley SW, Woodward AA (1993) The response of phimosis to local steroid application. Pediatr Surg Int 8:329–332
Gainder D (1949) The fate of the foreskin. BMJ 2:1433–1437
Rickwood AMK, Hemalatha V, Batcup G, Spitz L (1980) Phimosis in boys. Br J Urol 52:147–150
Kayaba H, Tamura H, Kitajima S, Fujiwara Y, Kato T, Kato T (1996) Analysis of shape and retractability of the prepuce in 603 japanese boys. J Urol 156:1813–1815
Zampieri N, Corroppolo M, Camoglio FS, Giacomello L, Ottolenghi A (2005) Phimosis: stretching methods with or without application of topical steroids? J Pediatr 147(5): 705–706
Miller JA, Munro DD (1980) Topical corticosteroids: clinical pharmacology and therapeutic use. Drugs 19:119–134
Brazzini B, Pimpinelli N (2002) New and established topical corticosteroids in dermatology: clinical pharmacology and therapeutic use. Am J Clin Dermatol 3:47–58
Rao LS, Long WS, Kaneko T, Blumenberg M (2003) Regulation of trascription factor activity by extracellular signals in epidermal keratinocytes. Acta Dermatoven 12:3–14
Radoja N, Nomine M, Jho SH, Blumenberg M, Tomic-canic M (2000) Novel mechanism of steroid action in skin through glucocorticoid receptor monomers. Mol Cell Biol 20:4328–4339
Austin RJH, Maschera B, Walker A, Fairbairn L, Meldrum E, Farrow SN, Uings IJ (2002) Mometasone fuorate is a less specific glucocorticoid than fluticonasone propionate. Eur Respir J 20:1386–1392
Croxtall JD, Paul-Clark M, Van Hall PTW (2003) Differential modulation of glucorticoid action by FK506 in A549 cells. Biochem J 376:285–290
Panarelli M, Holloway CD, Fraser R, Connell JMC, Ingram MC, Anderson NH, Kenyon CJ (1998) Glucorticoid receptor polymorphism, skin vasoconstriction and other metabolic intermediate phenotypes in normal human subjects. J Clin Endocrinol Metab 83:1846–1852
Bonacci JV, Harris T, Wilson JW, Stewart AG (2003) Collagen-induced resistance to glucocorticoid anti-mitogenic actions: a potential explanation of smooth muscle hyperplasia in the asthmatic remodeled airway. Br J Pharmacol 138:1203–1206
Oikarien A, Salo T, Ala-Kokko L, Tryggvason K (1987) Dexamethasone modulates the metabolism of type IV collagen and fidronectin in human basement-membrane-forming fibrosarcoma (HT-1080) cells. J Biochem 245:235–241
Barnes PJ (1998) Anti-inflammatory actions of glucocorticoids: molecular mechanisms. Clin Sci 94:557–572
Gysler A, Kleuser B, Sippl W, Lange K, Korting HC, Holtje HD, Schafer-Korting M (1999) Skin penetration and metabolism of topical glucocorticoids in reconstructed epidermis and in excised human skin. Pharm Res 16:1386–1391
Oikarinen A, Oikarinen H, Tan EM, Uitto J (1987) Modulation of collagen metabolism in cultured human skin fibroblasts by dexamethasone: correlation with glucocorticoid receptor density. Acta Derm Venereol 67:106–115
EFL (2005) Clinical potencies of glucocorticoids: what do we really measure? Curr Respir Med Rev 1:103–108
Bray PL, Du B, Mejia VM, Hao SC, Deutsch E, Fu C, Wilson RC, Hanauske-Abel H, McCaffrey TA (1999) Glucocorticoid resistance caused by reduced expression of the glucorticoid receptor in cells from human vascular lesions. Arterioscler Thromb Vasc Biol 19:1180–1189
Jefferson G, Lond MS, Victoria FRCS BC (1916) The peripenic muscle: some observations on the anatomy of phimosis. Surg Gynecol Obstet 23(2):177–181
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zampieri, N., Corroppolo, M., Zuin, V. et al. Phimosis and topical steroids: new clinical findings. Pediatr Surg Int 23, 331–335 (2007). https://doi.org/10.1007/s00383-007-1878-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-007-1878-x