Abstract
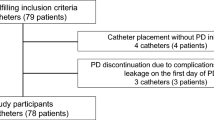
Despite advancements in catheter design and dialysis technique, catheter related complications still remain a common clinical problem in paediatric patients on chronic peritoneal dialysis (PD); in particular, infections are a common cause of patient’s morbidity and technique failure. In the present paper, data on 89 catheters implanted between January 1986 and December 2002 are reviewed to analyse the major causes of complications and/or PD failure and to ascertain their optimal management. A total of 89 catheters were implanted in 78 patients at the start of chronic PD: 26 in children under 2 years of age, 14 in children aged 2–5 years and 49 in patients over 5 years. Mean age of patients was 76.1 ± 73.0 months and median treatment time 14.5 ± 13.1 months. All catheters were surgically implanted and partial omentectomy was performed in 70% of cases. Straight Tenckhoff catheters were used in 70 cases (78%), curled ones in 19 (22%). Sixty-three catheters (71%) had two cuffs, 26 (29%) a single cuff. The entry-site was the midline in 34 patients (38%) and the paramedian line in 55 patients (62%). Catheter survival rate was 80% at 12 months, 62% at 24 months and 58% at 36 and 48 months, respectively. The incidence of catheter-related complications was one episode every 6.4 PD-months, and they were mainly represented by peritonitis (61%), exit-site infections and tunnel infection (ESI + TI: 23%), catheter obstruction (5%), dislocation (3.5%), leakage (2.5%). After the introduction of curled single-cuff catheters, a considerable reduction in the peritonitis incidence was observed during the last 7 years. A more prolonged catheter survival was observed in older children (>5 vs. <2 years: P < 0.05). Leakage was less common in catheters with paramedian entry-site compared with catheters implanted on the midline. In 7 out of 11 (64%) patients with catheter obstruction, omentectomy had not been performed. Single-cuff catheters had a lower infection-rate than double-cuff catheter (P < 0.01). Single cuff-curled Tenckhoff catheter can be considered the first choice catheter. Single cuff-catheters are not associated with an increase of infections. The surgical technique requires a strict adherence to a standardized procedure and a dedicated team, in order to obtain a reduction of the complications, a prolonged catheter duration and a better quality of life.

Similar content being viewed by others
Abbreviations
- PD:
-
Peritoneal dialysis
- ESI:
-
Exit-site infections
- TI:
-
Tunnel infection
- IC:
-
Infectious complications
References
Kuizon B, Melocoton TL, Holloway M, Ingles S, He-Jing, Fonkalsrud EW, Salusky IB (1995) Infectious and catheter-related complications in pediatric patients treated with peritoneal dualysis institution. Pediatr Nephrol 9:12–17
Schaefer F, Klaus G, Muller-Wiefel DE, Mehls O and the Mid European Pediatric Peritoneal Dialysis Study Group (MEPPS) (1999) Current practice of peritoneal dialysis in children: results of a longitudinal survey. Perit Dial Int 19(suppl 2):445–449
Furth SL, Donaldson LA, Sullivan EK, Watkins SL for the North American Pediatric Renal Transplant Cooperative Study (2000) Peritoneal dialysis catheter infections and peritonitis in children: a report of the North American Pediatric Renal Transplant Cooperative Study. Pediatr Nephrol 15:179–182
Warady BA (1988) Peritoneal dialysis catheter related infections in children. Pediatr Infect Dis J 17:1163–1166
Rinaldi S, Sera F, Verrina E, Edefonti A, Perfumo F, Sorino P, Zacchello G, Andreetta B, Ardissino G et al (1998) The Italian Registry of Pediatric Chronic Peritoneal Dialysis: a ten year experience with chronic peritoneal dialysis catheter. Perit Dial Int 18:71–74
Warady BA, Hebert D, Sullivan EK, Alexander SR, Tejani A (1997) Renal transplantation, chronic dialysis and chronic renal insufficiency in children and adolescents. The 1995 annual report of the North American Pediatric Renal Transplant Cooperative Study. Pediatr Nephrol 11:49–64
Warady BA et al (2000) ISPD guidelines/recommendations. Perit Dial Int 20:610–624
Pierratos A (1984) Peritoneal dialysis glossary. Perit Dial Bull 4:2–3
Ledermann SE, Scanes ME, Fernando ON, Duffy PG, Madden SJ, Trompeter RS (1999) Long-term outcome of peritoneal dialysis in infants. J Pediatr 136:24–29
Holley JL, Bernardini J, Piraino B (1994) Infecting organism in continuous ambulatory peritoneal dialysis patients on the Y-set. Am J Kidney Dis 23:569–573
Piraino B (1996) Exit-site care. Perit Dial Int 16(suppl 1):336–339
Honda M (1999). The 1997 report of the Japanese National Registry data on pediatric peritoneal dialysis patients. Perit Dial Int 19(2):473–478
Khanna R, Twardowski ZJ (1988) Peritoneal catheter exit-site (Editorial). Perit Dial Int 10:25–29
Helfrich GB, Winchester JF (1982) Shaving of external cuff of peritoneal catheter. Perit Dial Bull 2:183
Suh H, Wadhwa NK, Cabrala T (1995) Subcutaneous cuff removal in in persistent exit-site tunnel infections in peritoneal dialysis. Adv Perit Dial 11:157–159
Reissman P, Lyass S, Shiloni E, Rivkind A, Berlatzky Y (1998) Placement of a peritoneal dialysis catheter with routine omentectomy–does it prevent obstruction of the catheter? Eur J Surg 164:703–707
Rinaldi S, Sera F, Verrina E, Edefonti A, Gianoglio B, Perfumo F, Sorino P, Zacchello G et al (2004) Chronic peritoneal dialysis catheters in children: a fifteen-year experience of the Italian Registry of Pediatric Chronic Peritoneal Dialysis. Perit Dial Int 24:481–486
Washburn KK, Currier H, Salter KJ, Brandt ML (2004) Surgical technique for peritoneal dialysis catheter placement in the pediatric patient: a North American survey. Adv Perit Dial 20:218–221
Honda M, Litaka K, Kawaguchi H, Sakurak H, Shunji A, Takao K, Tuzuki K et al (1996) The Japanese Registry data on pediatric CAPD patients: a ten-year experience. Perit Dial Int 16:269–275
Stegmair B, Hedberg B, Sandzen B (1990) Absence of leakage by insertion o peritoneal dialysis catheter through the rectal muscle. Perit Dial Int 10:53–55
Leblanc M, Ouimet D, Pichette V (2001) Dialysate leaks in peritoneal dialysis. Semin Dial 14:50–54
Acknowledgments
The authors wish to thank the “Associazione per il Bambino Nefropatico” for its constant and kind collaboration. This study would not have been possible without the important technical and organizational contribution of Mario Scirocco.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Macchini, F., Valadè, A., Ardissino, G. et al. Chronic peritoneal dialysis in children: catheter related complications. A single centre experience. Ped Surgery Int 22, 524–528 (2006). https://doi.org/10.1007/s00383-006-1685-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-006-1685-9