Abstract
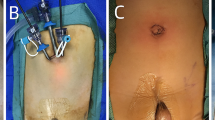
Our aim was to evaluate the utility of the high scrotal orchidopexy (Bianchi) approach for palpable undescended testis (UDT) and to assess long-term follow-up. We reviewed the records of orchidopexies performed between 1999 and 2002. The patients were then categorized by intraoperative exam under anesthesia as to whether their testes were palpable or nonpalpable. All palpable UDT that were initially thought to be amenable to a single high scrotal approach (Bianchi) were then reviewed. These cases were then analyzed to assess the impact of patient age, initial location of the testis, and prior inguinal/scrotal surgery with respect to the necessity to convert to a standard two-incision technique, and to analyze success and complications at 6–12-week and 1-year follow-up. Two hundred and nineteen orchidopexies were performed on 204 patients over this 4-year period. There were 178 testes palpable, and the transscrotal approach was used in 85 patients (100 orchidopexies). The preoperative positions of the testes that were thought to be amenable to Bianchi technique included the following: gliding (19), secondary trapped (25), superficial inguinal pouch (42), and location within the inguinal canal (2), while the remaining 12 testes were ectopic. Six patients required conversion to a traditional inguinal approach because of insufficient cord length via the single incision to allow the testis to lie in the scrotum. All patent processes vaginalis were ligated via the scrotal incision, regardless of their size. All patients, except for one who had a testis in the superficial inguinal pouch, had palpable testes of stable size and in a dependent position at 6–12-week follow-up. Of the 62 children who returned for 1-year follow-up, all had findings identical to those at their initial 6-week visits, with no atrophy or secondary reascent. Postoperative complications included transient postoperative scrotal hematoma in a single patient. The single failure underwent a successful two-incision orchidopexy for secondary reascent and a resultant trapped testis. Children with primary palpable undescended, gliding, or trapped testes can be managed successfully through the transscrotal route in the majority of cases. With use of a tailored approach to the palpable UDT, an additional groin incision is necessary only for a minority of appropriately selected cases.

Similar content being viewed by others
References
Schuller M (1881) On inguinal testicle and its operative treatment by transplanting into the scrotum. Ann Anat Surg 4:89–102
Bevan AD (1899) Operation on undescended testicle and congenital inguinal hernia. JAMA 33:773–777
Moul JW, Belman AB (1988) A review of surgical treatment of undescended testes with emphasis on anatomical position. J Urol 140:125–128
Spitz L (1988) Orchidopexy. In: Spitz L, Nixon NH (eds) Rob and Smith’s operative surgery, 4th edn. Butterworths, London, pp 603–608
Scorer CG, Farrington GH (1971) Congenital deformities of testes and epididymis. Appleton-Century-Crofts, New York
Bianchi A, Squire BR (1989) Transscrotal orchidopexy: orchidopexy revised. Pediatr Surg Int 4:189–192
Iyer KR, Kumar V, Huddart SN, et al. (1995) The scrotal approach. Pediatr Surg Int 10:58–60
Koyle MA, Walsh R, Caruso A, et al. (1999) Scrotal (Bianchi) approach to patent processus vaginalis in children. Tech Urol 5:95–96
Jackson MB, Chilvers C, Pike MC, et al. (1986) Cryptorchidism: an apparent substantial increase since 1960. Br Med J 293:1401–1404
Berkowitz GS, Lapinsky RH, Dolgin SE, et al. (1993) Prevalence and natural history of cryptorchidism. Pediatrics 92:44–49
Ritchey ML, Bloom DA (1995) Modified dartos pouch orchidopexy. Urology 45:136–138
Saha SK (1978) Cardopexy—a new approach to the undescended testes. Br J Urol 50:39–42
Caruso AP, Walsh RA, Koyle MA, et al. (2000) Single scrotal incision orchidopexy for the palpable undescended testicle. J Urol 164:156–159
Parsons JK, Ferrer F, Docimo SG (2003) The low scrotal approach to the ectopic or ascended testicle: prevalence of a patent processus vaginalis. J Urol 169:1832–1833
Maizels M, Gomez F, Firlit CF (1983) Surgical correction of the failed orchidopexy. J Urol 130:955
Cartwright PC, Velagapudi S, Snyder HM, et al. (1993) A surgical approach to reoperative orchidopexy. J Urol 149:817
Hutson JM, Goh DW (1993) Can undescended testes be acquired? Lancet 341:504
Docimo SG (1995) The results of surgical therapy for cryptorchidism: a literature review and analysis. J Urol 154:1148–1152
Eardley I, Saw KC, Whitaker RH (1994) Surgical outcome of orchidopexy. II. Trapped and ascended testes. Br J Urol 73:204
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rajimwale, A., Brant, W.O. & Koyle, M.A. High scrotal (Bianchi) single-incision orchidopexy: a “tailored” approach to the palpable undescended testis. Ped Surgery Int 20, 618–622 (2004). https://doi.org/10.1007/s00383-004-1243-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-004-1243-2