Abstract
Objective
To ascertain the presence of catatonia in cases of pediatric postoperative cerebellar mutism syndrome (PPCMS).
Method
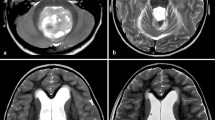
A systematic review of PPCMS case reports of patients aged 0–17 years with sufficient clinical information to extract catatonic phenomena was undertaken following PRISMA guidelines. Standardized catatonia rating scales were applied to selected cases retrospectively to ascertain whether diagnostic criteria for catatonia were met. A case known to the authors is also presented.
Results
Two hundred twenty-one suitable full-text articles were identified. Following screening and application of inclusion criteria, 51 articles were selected plus seven more from their references, reporting on 119 subjects. All cases met Bush and Francis (BF) diagnostic criteria for catatonia, 92.5% Pediatric Catatonia Rating Scale (PCRS), 52.9% ICD-11, and 44.5% DSM-5. All patients presented with mutism. The next most frequent signs were immobility/stupor (77.3%), withdrawal (35.3%), mannerisms (23.5%), and excitement/agitation (18.5%). Most cases presented with stuporous catatonia (75.6%). Catatonia most frequently occurred following resection of medulloblastoma (64.7%). Preoperative hydrocephalus occurred in 89 patients (74.8%).
Conclusion
Catatonia was frequent in this PPCMS sample, with a predominant stuporous variant; it should be considered in patients with PPCMS and assessed with reliable and validated instruments for prompt diagnosis and management.


Similar content being viewed by others
Data availability
No datasets were generated or analyzed during the current study.
References
Fink M (2013) Rediscovering catatonia: the biography of a treatable syndrome. Acta Psychiatr Scand 1:47. https://doi.org/10.1111/acps.12038
Benarous X, Raffin M, Ferrafiat V et al (2018) Catatonia in children and adolescents: new perspectives. Schizophr Res 200:56–67. https://doi.org/10.1016/j.schres.2017.07.028
Cohen D (2006) Towards a valid nosography and psychopathology of catatonia in children and adolescents. Int Rev Neurobiol 72:131–147. https://doi.org/10.1016/S0074-7742(05)72008-0
Cornic F, Consoli A, Tanguy M-L et al (2009) Association of adolescent catatonia with increased mortality and morbidity: evidence from a prospective follow-up study. Schizophr Res 113:233–240. https://doi.org/10.1016/j.schres.2009.04.021
Luccarelli J, Kalinich M, Fernandez-Robles C et al (2022) The incidence of catatonia diagnosis among pediatric patients discharged from general hospitals in the United States: a Kids’ Inpatient Database study. Front Psychiatry 13:878173. https://doi.org/10.3389/fpsyt.2022.878173
Rosebush PI, Mazurek MF (1999) Catatonia: re-awakening to a forgotten disorder. Mov Disord Off J Mov Disord Soc 14:395–397. https://doi.org/10.1002/1531-8257(199905)14:3%3c395::aid-mds1002%3e3.0.co;2-l
Cámara S, Fournier MC, Cordero P et al (2020) Neuropsychological profile in children with posterior fossa tumors with or without postoperative cerebellar mutism syndrome (CMS). Cerebellum Lond Engl 19:78–88. https://doi.org/10.1007/s12311-019-01088-4
Laustsen AF, Børresen ML, Hauerberg J, Juhler M (2023) Cerebellar mutism syndrome of non-tumour surgical aetiology-a case report and literature review. Childs Nerv Syst ChNS Off J Int Soc Pediatr Neurosurg 39:2201–2213. https://doi.org/10.1007/s00381-023-05947-8
Gudrunardottir T, Morgan AT, Lux AL et al (2016) Consensus paper on post-operative pediatric cerebellar mutism syndrome: the Iceland Delphi results. Childs Nerv Syst ChNS Off J Int Soc Pediatr Neurosurg 32:1195–1203. https://doi.org/10.1007/s00381-016-3093-3
Wickenhauser ME, Khan RB, Raches D et al (2020) Characterizing posterior fossa syndrome: a survey of experts. Pediatr Neurol 104:19–22. https://doi.org/10.1016/j.pediatrneurol.2019.11.007
Patel N, Keating G, Solanki GA et al (2023) Medulloblastomas, CNS embryonal tumors, and cerebellar mutism syndrome: advances in care and future directions. Childs Nerv Syst ChNS Off J Int Soc Pediatr Neurosurg 39:2633–2647. https://doi.org/10.1007/s00381-023-06112-x
Noris A, Zicca A, Lenge M et al (2021) The medical therapy for cerebellar mutism syndrome: a case report and literature review. Childs Nerv Syst ChNS Off J Int Soc Pediatr Neurosurg 37:2727–2734. https://doi.org/10.1007/s00381-021-05233-5
Moher D, Liberati A, Tetzlaff J et al (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 62:1006–1012. https://doi.org/10.1016/j.jclinepi.2009.06.005
Benarous X, Consoli A, Raffin M et al (2016) Validation of the Pediatric Catatonia Rating Scale (PCRS). Schizophr Res 176:378–386. https://doi.org/10.1016/j.schres.2016.06.020
Sienaert P, Rooseleer J, De Fruyt J (2011) Measuring catatonia: a systematic review of rating scales. J Affect Disord 135:1–9. https://doi.org/10.1016/j.jad.2011.02.012
Wortzel J, Oldham M (2022) Bush-Francis Catatonia Rating Scale training manual and coding guide. https://www.urmc.rochester.edu/MediaLibraries/URMCMedia/psychiatry/documents/BFCRS-Training-Manual-22-02-24.pdf
Bush G, Fink M, Petrides G et al (1996) Catatonia. I. Rating scale and standardized examination. Acta Psychiatr Scand 93:129–136. https://doi.org/10.1111/j.1600-0447.1996.tb09814.x
American Psychiatric Association, DSM-5 Task Force (2013) Diagnostic and statistical manual of mental disorders: DSM-5™ (5th ed.). American Psychiatric Publishing, Inc.
Reed GM, First MB, Kogan CS et al (2019) Innovations and changes in the ICD-11 classification of mental, behavioural and neurodevelopmental disorders. World Psychiatry Off J World Psychiatr Assoc WPA 18:3–19. https://doi.org/10.1002/wps.20611
Aguiar PH, Plese JP, Ciquini O, Marino R (1995) Transient mutism following a posterior fossa approach to cerebellar tumors in children: a critical review of the literature. Childs Nerv Syst ChNS Off J Int Soc Pediatr Neurosurg 11:306–310. https://doi.org/10.1007/BF00301766
Akhaddar A, Salami M, El Asri AC, Boucetta M (2012) Treatment of postoperative cerebellar mutism with fluoxetine. Childs Nerv Syst ChNS Off J Int Soc Pediatr Neurosurg 28:507–508. https://doi.org/10.1007/s00381-012-1719-7
Alharbi S, Bawazir M, Altweijri I (2022) A case of postoperative cerebellar mutism with hyperphagia in a child following gross total resection of medulloblastoma occupying the cerebellar vermis. Childs Nerv Syst ChNS Off J Int Soc Pediatr Neurosurg 38:2189–2198. https://doi.org/10.1007/s00381-022-05520-9
Al-Jarallah A, Cook JD, Gascon G et al (1994) Transient mutism following posterior fossa surgery in children. J Surg Oncol 55:126–131. https://doi.org/10.1002/jso.2930550214
Amor-García MÁ, Fernández-Llamazares CM, Manrique-Rodríguez S et al (2021) Bromocriptine for the treatment of postoperative cerebellar mutism syndrome in pediatric patients: three case reports. J Oncol Pharm Pract Off Publ Int Soc Oncol Pharm Pract 27:1753–1757. https://doi.org/10.1177/1078155220982046
Arai Y, Okanishi T, Oguri M et al (2022) Power and connectivity changes on electroencephalogram in postoperative cerebellar mutism. Brain Dev 44:759–764. https://doi.org/10.1016/j.braindev.2022.06.006
Asamoto M, Ito H, Suzuki N et al (1994) Transient mutism after posterior fossa surgery. Childs Nerv Syst ChNS Off J Int Soc Pediatr Neurosurg 10:275–278. https://doi.org/10.1007/BF00301168
Bhatoe HS (1997) Mutism, oropharyngeal apraxia and dysarthria after posterior fossa tumour excision. Br J Neurosurg 11:341–343. https://doi.org/10.1080/02688699746140
Catsman-Berrevoets CE, Van Dongen HR, Aarsen FK, Paquier PF (2003) Transient cerebellar eye closure and mutism after cerebellar tumor surgery: long-term clinical follow-up of neurologic and behavioral disturbances in a 14-year-old girl. Pediatr Neurosurg 38:122–127. https://doi.org/10.1159/000068816
Catsman-Berrevoets CE, Aarsen FK (2010) The spectrum of neurobehavioural deficits in the posterior fossa syndrome in children after cerebellar tumour surgery. Cortex J Devoted Study Nerv Syst Behav 46:933–946. https://doi.org/10.1016/j.cortex.2009.10.007
Chao JY, Liu C, Shetty N, Shah U (2017) Postoperative pediatric cerebellar mutism after posterior fossa surgery. Case Rep 8:213–215. https://doi.org/10.1213/XAA.0000000000000467
Clerico A, Sordi A, Ragni G et al (2002) Brief report: Transient mutism following posterior fossa surgery studied by single photon emission computed tomography (SPECT). Med Pediatr Oncol 38:445–448. https://doi.org/10.1002/mpo.1361
Dailey AT, McKhann GM, Berger MS (1995) The pathophysiology of oral pharyngeal apraxia and mutism following posterior fossa tumor resection in children. J Neurosurg 83:467–475. https://doi.org/10.3171/jns.1995.83.3.0467
Daniels SR, Moores LE, DiFazio MP (2005) Visual disturbance associated with postoperative cerebellar mutism. Pediatr Neurol 32:127–130. https://doi.org/10.1016/j.pediatrneurol.2004.07.014
De Witte E, Wilssens I, De Surgeloose D et al (2017) Apraxia of speech and cerebellar mutism syndrome: a case report. Cerebellum Ataxias 4:2. https://doi.org/10.1186/s40673-016-0059-x
Dietze DD, Mickle JP (1990) Cerebellar mutism after posterior fossa surgery. Pediatr Neurosurg 16:25–31; discussion 31. https://doi.org/10.1159/000120499
Di Cataldo A, Dollo C, Astuto M et al (2001) Mutism after surgical removal of a cerebellar tumor: two case reports. Pediatr Hematol Oncol 18:117–121. https://doi.org/10.1080/088800101300002946
Ferrante L, Mastronardi L, Acqui M, Fortuna A (1990) Mutism after posterior fossa surgery in children. Report of three cases J Neurosurg 72:959–963. https://doi.org/10.3171/jns.1990.72.6.0959
García Conde M, Martín Viota L, FeblesGarcía P et al (2007) Mutismo cerebeloso grave tras cirugía de un tumor de fosa posterior. An Pediatría 66:75–79. https://doi.org/10.1157/13097364
Gaskill SJ, Marlin AE (1991) Transient eye closure after posterior fossa tumor surgery in children. Pediatr Neurosurg 17:196–198. https://doi.org/10.1159/000120595
Gedik GK, Sari O, Köktekir E, Akdemir G (2017) Fluorodeoxyglucose positron emission tomography/computed tomography findings in a patient with cerebellar mutism after operation in posterior fossa. Asian J Surg 40:166–170. https://doi.org/10.1016/j.asjsur.2014.01.004
Germanò A, Baldari S, Caruso G et al (1998) Reversible cerebral perfusion alterations in children with transient mutism after posterior fossa surgery. Childs Nerv Syst ChNS Off J Int Soc Pediatr Neurosurg 14:114–119. https://doi.org/10.1007/s003810050191
Gorker I, Cobanoglu S, San V (2012) A case of cerebellar mutism after posterior fossa surgery. Arch Neuropsychiatry 49:320–323
Gündüz HB, Yassa MİK, Ofluoğlu AE et al (2013) Cerebellar mutism syndrome after posterior fossa surgery: a report of two cases of pilocytic astrocytoma. Noro Psikiyatri Arsivi 50:368–371. https://doi.org/10.4274/npa.y6311
Herb E, Thyen U (1992) Mutism after cerebellar medulloblastoma surgery. Neuropediatrics 23:144–146. https://doi.org/10.1055/s-2008-1071330
Ichinose M, Abe M, Hirotsu T, Tabuchi K (1997) Sequential SPECT analysis of cerebellar mutism after removal of medulloblastoma: a case report. Jpn J Neurosurg 6:493–497. https://doi.org/10.7887/jcns.6.493
Ishibashi T, Nagahima H, Takahashi K et al (1998) Cerebellar mutism after posterior fossa surgery in the child : a case report. Jpn J Neurosurg 7:591–595. https://doi.org/10.7887/jcns.7.591
Jones S, Kirollos RW, Van Hille PT (1996) Cerebellar mutism following posterior fossa tumour surgery. Br J Neurosurg 10:221–224. https://doi.org/10.1080/02688699650040421
Kalelioglu M, Isik N, Isik N, Sarier M (1995) Mutism after total removal of medulloblastoma: case report. Turk Neurosurg 5:62–64
Kingma A, Mooij JJ, Metzemaekers JD, Leeuw JA (1994) Transient mutism and speech disorders after posterior fossa surgery in children with brain tumours. Acta Neurochir (Wien) 131:74–79. https://doi.org/10.1007/BF01401456
Lanier JC, Abrams AN (2017) Posterior fossa syndrome: review of the behavioral and emotional aspects in pediatric cancer patients. Cancer 123:551–559. https://doi.org/10.1002/cncr.30238
Liu GT (1998) Visual impairment associated with mutism after posterior fossa surgery in children. Neurosurgery 43:983
Mortimer DS (2011) Clinical case study: a 4-year-old boy with posterior fossa syndrome after resection of a medulloblastoma. J Neurosci Nurs J Am Assoc Neurosci Nurses 43:225–229. https://doi.org/10.1097/JNN.0b013e3182212af9
Moshref R, Mirdad A (2021) Cerebellar mutism treated successfully with zolpidem in a patient with learning difficulties. Cureus 13:e16616. https://doi.org/10.7759/cureus.16616
Nicita F, Paiano M, Liberatore M et al (2017) Sudden benzodiazepine-induced resolution of post-operative pediatric cerebellar mutism syndrome: a clinical-SPECT study. Acta Neurochir (Wien) 159:475–479. https://doi.org/10.1007/s00701-016-3059-y
Ozimek A, Richter S, Hein-Kropp C et al (2004) Cerebellar mutism–report of four cases. J Neurol 251:963–972. https://doi.org/10.1007/s00415-004-0472-6
Pollack IF, Polinko P, Albright AL et al (1995) Mutism and pseudobulbar symptoms after resection of posterior fossa tumors in children: incidence and pathophysiology. Neurosurgery 37:885–893. https://doi.org/10.1227/00006123-199511000-00006
Prol P, Alaniz Y, Sbruzzi A et al (2021) Síndrome de mutismo cerebeloso en pediatría. Reporte de un caso Neurol Argent 13:131–134. https://doi.org/10.1016/j.neuarg.2021.05.002
Rekate HL, Grubb RL, Aram DM et al (1985) Muteness of cerebellar origin. Arch Neurol 42:697–698. https://doi.org/10.1001/archneur.1985.04060070091023
Ross SG, Northman L, Morris M et al (2014) Cerebellar mutism after posterior fossa tumor resection: case discussion and recommendations for psychoeducational intervention. J Pediatr Oncol Nurs Off J Assoc Pediatr Oncol Nurses 31:78–83. https://doi.org/10.1177/1043454213518975
Siffert J, Poussaint TY, Goumnerova LC et al (2000) Neurological dysfunction associated with postoperative cerebellar mutism. J Neurooncol 48:75–81. https://doi.org/10.1023/a:1006483531811
Sordyl R, Schroter M, Rosol I et al (2023) Transient improvement of the postoperative pediatric cerebellar mutism syndrome following intravenous midazolam injection. Interdiscip Neurosurg 31:101683. https://doi.org/10.1016/j.inat.2022.101683
Stein BM, Tenner MS, Fraser RAR (1972) Hydrocephalus following removal of cerebellar astrocytomas in children. J Neurosurg 36:763–768. https://doi.org/10.3171/jns.1972.36.6.0763
Vandeinse D, Hornyak JE (1997) Linguistic and cognitive deficits associated with cerebellar mutism. Pediatr Rehabil 1:41–44. https://doi.org/10.3109/17518429709060941
van Dongen HR, Catsman-Berrevoets CE, van Mourik M (1994) The syndrome of “cerebellar” mutism and subsequent dysarthria. Neurology 44:2040–2046. https://doi.org/10.1212/wnl.44.11.2040
van Mourik M, Catsman-Berrevoets CE, van Dongen HR, Neville BG (1997) Complex orofacial movements and the disappearance of cerebellar mutism: report of five cases. Dev Med Child Neurol 39:686–690. https://doi.org/10.1111/j.1469-8749.1997.tb07364.x
da Wagner RC, Gallo P, Oppitz PP (1995) Mudez após cirurgia para tumor da fossa posterior relato de dois casos. Arq. Neuro-Psiquiatr. 53(3A):533–534
Walker D, Thomas SA, Talbot EJ et al (2014) Cerebellar mutism: the rehabilitation challenge in pediatric neuro-oncology: case studies. J Pediatr Rehabil Med 7:333–340. https://doi.org/10.3233/PRM-140309
Wisoff JH, Epstein FJ (1984) Pseudobulbar palsy after posterior fossa operation in children. Neurosurgery 15:707–709. https://doi.org/10.1227/00006123-198411000-00014
Catsman-Berrevoets CE, van Dongen HR, Zwetsloot CP (1992) Transient loss of speech followed by dysarthria after removal of posterior fossa tumour. Dev Med Child Neurol 34:1102–1109. https://doi.org/10.1111/j.1469-8749.1992.tb11424.x
Daly DD, Love JG (1958) Akinetic mutism. Neurology 8:238–242. https://doi.org/10.1212/wnl.8.3.238
Küpeli S, Yalçın B, Bilginer B et al (2011) Posterior fossa syndrome after posterior fossa surgery in children with brain tumors. Pediatr Blood Cancer 56:206–210. https://doi.org/10.1002/pbc.22730
Kusano Y, Tanaka Y, Takasuna H et al (2006) Transient cerebellar mutism caused by bilateral damage to the dentate nuclei after the second posterior fossa surgery. Case report J Neurosurg 104:329–331. https://doi.org/10.3171/jns.2006.104.2.329
Nagatani K, Waga S, Nakagawa Y (1991) Mutism after removal of a vermian medulloblastoma: cerebellar mutism. Surg Neurol 36:307–309. https://doi.org/10.1016/0090-3019(91)90094-P
Pollack IF (1997) Posterior fossa syndrome. In: Schmahmann JD (ed) International review of neurobiology. Academic Press, pp 411–432
Steinbok P, Cochrane DD, Perrin R, Price A (2003) Mutism after posterior fossa tumour resection in children: incomplete recovery on long-term follow-up. Pediatr Neurosurg 39:179–183. https://doi.org/10.1159/000072468
Grover S, Chauhan N, Sharma A et al (2017) Symptom profile of catatonia in children and adolescents admitted to psychiatry inpatient unit. Asian J Psychiatry 29:91–95. https://doi.org/10.1016/j.ajp.2017.04.016
Thakur A, Jagadheesan K, Dutta S, Sinha VK (2003) Incidence of catatonia in children and adolescents in a paediatric psychiatric clinic. Aust N Z J Psychiatry 37:200–203. https://doi.org/10.1046/j.1440-1614.2003.01125.x
Cohen D, Nicolas J-D, Flament MF et al (2005) Clinical relevance of chronic catatonic schizophrenia in children and adolescents: evidence from a prospective naturalistic study. Schizophr Res 76:301–308. https://doi.org/10.1016/j.schres.2005.01.014
Dhossche DM, Bouman NH (1997) Catatonia in an adolescent with Prader-Willi syndrome. Ann Clin Psychiatry Off J Am Acad Clin Psychiatr 9:247–253. https://doi.org/10.1023/a:1022308511313
Northoff G, Koch A, Wenke J et al (1999) Catatonia as a psychomotor syndrome: a rating scale and extrapyramidal motor symptoms. Mov Disord Off J Mov Disord Soc 14:404–416. https://doi.org/10.1002/1531-8257(199905)14:3%3c404::aid-mds1004%3e3.0.co;2-5
Carroll BT, Kirkhart R, Ahuja N et al (2008) Katatonia Psychiatry Edgmont 5:42–50
Kahlbaum KL (1973) Catatonia. (Trans Levij Y, Pridan T) The Johns Hopkins University Press, Baltimore, MD
Boisgontier J, Beccaria K, Saitovitch A et al (2023) Case report: zolpidem’s paradoxical restorative action: a case report of functional brain imaging. Front Neurosci 17. https://doi.org/10.3389/fnins.2023.1127542
Oldham MA (2022) Describing the features of catatonia: a comparative phenotypic analysis. Schizophr Res S0920–9964(22):00294–00298. https://doi.org/10.1016/j.schres.2022.08.002
Stuivenga M, Morrens M (2014) Prevalence of the catatonic syndrome in an acute inpatient sample. Front Psychiatry 5:174. https://doi.org/10.3389/fpsyt.2014.00174
Jaimes-Albornoz W, Ruiz de Pellon-Santamaria A, Nizama-Vía A et al (2022) Catatonia in older adults: a systematic review. World J Psychiatry 12:348–367. https://doi.org/10.5498/wjp.v12.i2.348
Dhossche DM, Wachtel LE (2010) Catatonia is hidden in plain sight among different pediatric disorders: a review article. Pediatr Neurol 43:307–315. https://doi.org/10.1016/j.pediatrneurol.2010.07.001
Dhossche D, Cohen D, Ghaziuddin N et al (2010) The study of pediatric catatonia supports a home of its own for catatonia in DSM-5. Med Hypotheses 75:558–560. https://doi.org/10.1016/j.mehy.2010.07.029
Denysenko L, Sagot A (2017) Post-surgical cerebellar mutism and catatonia. Acta Neurochir (Wien) 159:1253–1254. https://doi.org/10.1007/s00701-017-3172-6
Rogers JP, Oldham MA, Fricchione G et al (2023) Evidence-based consensus guidelines for the management of catatonia: recommendations from the British Association for Psychopharmacology. J Psychopharmacol Oxf Engl 37:327–369. https://doi.org/10.1177/02698811231158232
Hauptman AJ, Benjamin S (2016) The differential diagnosis and treatment of catatonia in children and adolescents. Harv Rev Psychiatry 24:379–395. https://doi.org/10.1097/HRP.0000000000000114
Acknowledgements
The authors would like to thank the patient and her family for allowing the use of their clinical information.
Author information
Authors and Affiliations
Contributions
Conceptualization: W.J.-A. and J.S.-M. Methodology: W.J.-A., J.S.-M., and M.I. Validation: W.J.-A., J.S.-M., P.W., L.G.M.-M.I., F.R., M.M.-Q., R.S., M.I., and A.R.P.S. Search strategy and database search: M.I. Formal analysis: W.J.-A., J.S.-M., P.W., L.G.M.-M.I., F.R., M.M.-Q., R.S., M.I., and A.R.P.S. Data curation: W.J.-A., J.S.-M., P.W., L.G.M.-M.I., F.R., M.M.-Q., R.S., M.I., and A.R.P.S. Writing–original draft preparation: W.J.-A., J.S.-M., P.W., L.G.M.-M.I., F.R., M.M.-Q., R.S., M.I., and A.R.P.S. Writing, review, and editing: W.J.-A., J.S.-M., P.W., L.G.M.-M.I., F.R., M.M.-Q., R.S., M.I., and A.R.P.S. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Disclaimer
We declare that this material has not been published previously in any form.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jaimes-Albornoz, W., Wu, P., de Mendaza-Martínez de Icaya, L.G. et al. Catatonia associated with pediatric postoperative cerebellar mutism syndrome. Childs Nerv Syst (2024). https://doi.org/10.1007/s00381-024-06392-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00381-024-06392-x