Abstract
Objective
Preventative protocols have efficaciously reduced shunt infection in developed countries. However, the generalizability of these protocols in low-to-middle-income countries (LMICs) remains unclear. Previously, shunt insertion in the authors’ center was routinely performed under institutional preventative precautions, which was updated via merging with the Hydrocephalus Clinical Research Network (HCRN) protocol. This study aimed to investigate the ventriculoperitoneal shunt (VPS) infection rates in pediatric patients following the implementation of the adapted protocol.
Methods
The adapted protocol was implemented in all first-time VPS implantations between 2011 and 2021. The primary outcome was a 6-month shunt infection. The Pearson chi-square test was used for categorical variables and the Mann-Whitney U-test for numeric variables to evaluate the correlation with shunt infection.
Results
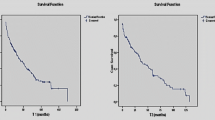
A total of 352 first-time VPS procedures were performed adhering to the adapted protocol. The median age was 5 months, and 189 (53.7%) were male. Overall, 37 patients (10.5%) experienced shunt infection, with 30 (8.5%) occurring within the first 6 months, which was lower than 13.3% infection rate of the previous series of the same center. The infection rate was slightly higher than the 5.7% and 6.0% rates reported by HCRN studies. Patients with shunt infection were significantly younger (7.5 versus 17.5 months, P < 0.001).
Conclusions
This study validates the efficacy of an adapted perioperative protocol in mitigating shunt infection in a high-volume center in a LMIC. Adhering to a step-by-step protocol, modified to suit the healthcare resources and financial constraints of LMICs, could maintain low shunt infection rates that are roughly comparable to those of centers in high-income countries.


Similar content being viewed by others
Availability of data and material
Queries about the data should be directed to the corresponding author.
References
Simon TD, Butler J, Whitlock KB, Browd SR, Holubkov R, Kestle JR, Kulkarni AV, Langley, Limbrick Jr DD, Mayer-Hamblett N, Tamber M (2014) Risk factors for first cerebrospinal fluid shunt infection: findings from a multi-center prospective cohort study. J Pediatr 164:1462–1468
Tamber MS, Klimo P, Mazzola CA, Flannery AM (2014) Pediatric hydrocephalus: systematic literature review and evidence-based guidelines. Part 8: Management of cerebrospinal fluid shunt infection. J Neurosurg Pediatr 14:60–71
González S, Carbonaro M, Fedullo AG, Sormani MI, Ceinos MD, Biochemistb RG, Rosanova MT (2018) Cerebrospinal fluid shunt-associated infections in pediatrics: Analysis of the epidemiology and mortality risk factors. Arch Argent Pediatr 116:198–203
Vinchon M, Dhellemmes P (2006) Cerebrospinal fluid shunt infection: risk factors and long-term follow-up. Childs Nerv Syst 22:692–697
Sciubba DM, Lin L-M, Woodworth GF, McGirt MJ, Carson B, Jallo GI (2007) Factors contributing to the medical costs of cerebrospinal fluid shunt infection treatment in pediatric patients with standard shunt components compared with those in patients with antibiotic-impregnated components. Neurosurg Focus 22:1–4
Kestle JR, Garton HJ, Whitehead WE, Drake JM, Kulkarni AV, Cochrane DD, Muszynski C, Walker ML (2006) Management of shunt infections: a multicenter pilot study. J Neurosurg Pediatr 105:177–181
Simon TD, Hall M, Dean JM, Kestle JRW, Riva-Cambrin J (2010) Reinfection following initial cerebrospinal fluid shunt infection. J Neurosurg Pediatr 6:277–285
Simon TD, Kronman MP, Whitlock KB, Gove NE, Mayer-Hamblett N, Browd SR, Cochrane DD, Holubkov R, Kulkarni AV, Langley M (2018) Reinfection after treatment of first cerebrospinal fluid shunt infection: a prospective observational cohort study. J Neurosurg Pediatr 21:346–358
Kestle JRW, Holubkov R, Cochrane DD, Kulkarni AV, Limbrick DD, Luerssen TG, Oakes WJ, Riva-Cambrin J, Rozzelle C, Simon TD (2016) A new Hydrocephalus Clinical Research Network protocol to reduce cerebrospinal fluid shunt infection. J Neurosurg Pediatr 17:391–396
Kestle JRW, Riva-Cambrin J, Wellons JC, Kulkarni AV, Whitehead WE, Walker ML, Oakes WJ, Drake JM, Luerssen TG, Simon TD (2011) A standardized protocol to reduce cerebrospinal fluid shunt infection: the Hydrocephalus Clinical Research Network Quality Improvement Initiative. J Neurosurg Pediatr 8:22–29
Omrani O, O’Connor J, Hartley J, James G (2018) Effect of introduction of a standardised peri-operative protocol on CSF shunt infection rate: a single-centre cohort study of 809 procedures. Childs Nerv Syst 34:2407–2414
Yang MMH, Hader W, Bullivant K, Brindle M, Riva-Cambrin J (2019) Calgary Shunt Protocol, an adaptation of the Hydrocephalus Clinical Research Network shunt protocol, reduces shunt infections in children. J Neurosurg Pediatr 23:559–567
Simon TD, Riva-Cambrin J, Srivastava R, Bratton SL, Dean JM, Kestle JRW (2008) Hospital care for children with hydrocephalus in the United States: utilization, charges, comorbidities, and deaths. J Neurosurg Pediatr 1:131–137
Leaper DJ, Edmiston CE (2017) World Health Organization: global guidelines for the prevention of surgical site infection. J Hosp Infect 95:135–136
Chu J, Jensen H, Holubkov R, Krieger MD, Kulkarni AV, Riva-Cambrin J, Rozzelle CJ, Limbrick DD, Wellons JC, Browd SR (2022) The Hydrocephalus Clinical Research Network quality improvement initiative: the role of antibiotic-impregnated catheters and vancomycin wound irrigation. J Neurosurg Pediatr 29:711–718
Nejat F, Tajik P, Ghodsi SM, Golestan B, Majdzadeh R, Yazdani S, Ansari S, Dadmehr M, Ganji S, Najafi M (2008) Breastfeeding: a potential protective factor against ventriculoperitoneal shunt infection in young infants. J Neurosurg Pediatr 1:138–141
Erps A, Roth J, Constantini S, Lerner-Geva L, Grisaru-Soen G (2018) Risk factors and epidemiology of pediatric ventriculoperitoneal shunt infection. Pediatr Int 60:1056–1061
Choux M, Genitori L, Lang D, Lena G (1992) Shunt implantation: reducing the incidence of shunt infection. J Neurosurg 77:875–880
Faillace WJ (1995) A no-touch technique protocol to diminish cerebrospinal fluid shunt infection. Surg Neurol 43:344–350
Pirotte BJM, Lubansu A, Bruneau M, Loqa C, Van Cutsem N, Brotchi J (2007) Sterile surgical technique for shunt placement reduces the shunt infection rate in children: preliminary analysis of a prospective protocol in 115 consecutive procedures. Childs Nerv Syst 23:1251–1261
Rotim K, Miklic P, Paladino J, Melada A, Marcikic M, Scap M (1997) Reducing the incidence of infection in pediatric cerebrospinal fluid shunt operations. Childs Nerv Syst 13:584–587
Spader HS, Hertzler DA, Kestle JRW, Riva-Cambrin J (2015) Risk factors for infection and the effect of an institutional shunt protocol on the incidence of ventricular access device infections in preterm infants. J Neurosurg Pediatr 15:156–160
Turner RS (1974) Laminar air flow: its original surgical application and long-term results. JBJS 56:430–435
Weiser MC, Moucha CS (2018) Operating-room airflow technology and infection prevention. JBJS 100:795–804
Larsson J, Sutherland S, Söderström Å, Roman-Emanuel C, Jeppsson A, Olofsson EH, Svensson P-A (2015) Bacterial contamination of suction catheter tips during aortic valve replacement surgery: a prospective observational cohort study. Patient Saf Surg 9:1–5
Robinson AH, Drew S, Anderson J, Bentley G, Ridgway GL (1993) Suction tip contamination in the ultraclean-air operating theatre. Ann R Coll Surg Engl 75:254
Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR, Committee HICPA (1999) Guideline for prevention of surgical site infection, 1999. Infect Control Hosp Epidemiol 20:247–280
Darouiche RO, Wall MJ Jr, Itani KMF, Otterson MF, Webb AL, Carrick MM, Miller HJ, Awad SS, Crosby CT, Mosier MC (2010) Chlorhexidine–alcohol versus povidone–iodine for surgical-site antisepsis. N Engl J Med 362:18–26
Mimoz O, Lucet J-C, Kerforne T, Pascal J, Souweine B, Goudet V, Mercat A, Bouadma L, Lasocki S, Alfandari S (2015) Skin antisepsis with chlorhexidine–alcohol versus povidone iodine–alcohol, with and without skin scrubbing, for prevention of intravascular-catheter-related infection (CLEAN): an open-label, multicentre, randomised, controlled, two-by-two factorial trial. Lancet 386:2069–2077
Muram S, Isaacs AM, Sader N, Holubkov R, Fong A, Conly J, Hamilton MG (2022) A standardized infection prevention bundle for reduction of CSF shunt infections in adult ventriculoperitoneal shunt surgery performed without antibiotic-impregnated catheters. J Neurosurg 1:1–9
Okamura Y, Maruyama K, Fukuda S, Horikawa H, Sasaki N, Noguchi A, Nagane M, Shiokawa Y (2019) Detailed standardized protocol to prevent cerebrospinal fluid shunt infection. J Neurosurg 132:755–759
Classen DC, Evans RS, Pestotnik SL, Horn SD, Menlove RL, Burke JP (1992) The timing of prophylactic administration of antibiotics and the risk of surgical-wound infection. N Engl J Med 326:281–286
Brown EM (1993) Antimicrobial prophylaxis in neurosurgery. J Antimicrob Chemother 31:49–63
Lee FH, Pfeffer M, Van Harken DR, Smyth RD, Hottendorf GH (1980) Comparative pharmacokinetics of ceforanide (BL-S786R) and cefazolin in laboratory animals and humans. Antimicrob Agents Chemother 17:188–192
Gathura E, Poenaru D, Bransford R, Albright AL (2010) Outcomes of ventriculoperitoneal shunt insertion in Sub-Saharan Africa. J Neurosurg Pediatr 6:329–335
Lane JD, Mugamba J, Ssenyonga P, Warf BC (2014) Effectiveness of the Bactiseal Universal Shunt for reducing shunt infection in a sub-Saharan African context: a retrospective cohort study in 160 Ugandan children. J Neurosurg Pediatr 13:140–144
Warf BC (2005) Comparison of 1-year outcomes for the Chhabra and Codman-Hakim Micro Precision shunt systems in Uganda: a prospective study in 195 children. J Neurosurg Pediatr 102:358–362
Dallacasa P, Dappozzo A, Galassi E, Sandri F, Cocchi G, Masi M (1995) Cerebrospinal fluid shunt infections in infants. Childs Nerv Syst 11:643–649
Forward KR, Fewer HD, Stiver HG (1983) Cerebrospinal fluid shunt infections: a review of 35 infections in 32 patients. J Neurosurg 59:389–394
McGirt MJ, Zaas A, Fuchs HE, George TM, Kaye K, Sexton DJ (2003) Risk factors for pediatric ventriculoperitoneal shunt infection and predictors of infectious pathogens. Clin Infect Dis 36:858–862. https://doi.org/10.1086/368191
Caceres A, Avila ML, Herrera ML (2018) Fungal infections in pediatric neurosurgery. Childs Nerv Syst 34:1973–1988
Adams DJ, Rajnik M (2014) Microbiology and treatment of cerebrospinal fluid shunt infections in children. Curr Infect Dis Rep 16:427. https://doi.org/10.1007/s11908-014-0427-8
Montero A, Romero J, Vargas JA, Regueiro CA, Sanchez-Aloz G, De Prados F, De la Torre A, Aragon G (2000) Candida infection of cerebrospinal fluid shunt devices: report of two cases and review of the literature. Acta Neurochir (Wien) 142:67–74
Author information
Authors and Affiliations
Contributions
A. Sh., acquisition of data, analysis and interpretation of data, drafting the manuscript; P. J., revising the manuscript; K.T. M., conception and design of the work, revising the manuscript; F. N., checking all aspects of the work in ensuring the accuracy or integrity of any part of the work; Z. H., conception and design of the work, checking all aspects of the work in ensuring the accuracy or integrity of any part of the work, final approval of the version to be published. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval
Institutional ethical approval code: IR.TUMS.CHMC.REC.1400.183. The study adhered to the tenets of the Declaration of Helsinki.
Consent to participate
Informed consent to use clinical data for research purposes had been taken from parents at admission time.
Consent for publication
Consent for publication was taken from parents, conditioning that the patients’ identity is not recognizable.
Conflict of interest
The authors have no conflict of interest/competing interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shahbandi, A., Jahangiri, P., Meybodi, K.T. et al. Implementation of an adapted perioperative ventriculoperitoneal shunting protocol in a tertiary center located in a low-to-middle-income country. Childs Nerv Syst (2024). https://doi.org/10.1007/s00381-024-06374-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00381-024-06374-z