Abstract
Introduction
Intraventricular hemorrhage (IVH) can ensue permanent neurologic dysfunction, morbidity, and mortality. While previous reports have identified disparities based on patient gender or weight, no prior study has assessed how race may influence in neonatal or infantile IVH patients. The aim of this study was to investigate the impact of race on adverse event (AE) rates, length of stay (LOS), and total cost of admission among newborns with IVH.
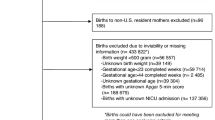
Methods
Using the 2016–2019 National Inpatient Sample database, newborns diagnosed with IVH were identified using ICD-10-CM codes. Patients were stratified based on race. Patient characteristics and inpatient outcomes were assessed. Multivariate logistic regression analyses were used to identify the impact of race on extended LOS and exorbitant cost.
Results
Of 1435 patients, 650 were White (45.3%), 270 African American (AA) (18.8%), 300 Hispanic (20.9%), and 215 Other (15.0%). A higher percentage of AA and Other patients than Hispanic and White patients were < 28 days old (p = 0.008). Each of the cohorts had largely similar presenting comorbidities and symptoms, although AA patients did have significantly higher rates of NEC (p < 0.001). There were no observed differences in rates of AEs, rates of mortality, mean LOS, or mean total cost of admission. Similarly, on multivariate analysis, no race was identified as a significant independent predictor of extended LOS or exorbitant cost.
Conclusions
Our study found that in newborns with IVH, race is not associated with proxies of poor healthcare outcomes like prolonged LOS or excessive cost. Further studies are needed to validate these findings.
Similar content being viewed by others
Data availability
No datasets were generated or analysed during the current study.
References
Papanicolas I, Woskie LR, Jha AK (2018) Health care spending in the United States and other high-income countries. JAMA 319(10):1024–1039. https://doi.org/10.1001/jama.2018.1150
Berwick DM, Nolan TW, Whittington J (2008) The triple aim: care, health, and cost. Health Aff (Millwood) 27(3):759–69. https://doi.org/10.1377/hlthaff.27.3.759
Mercer MP, Singh MK, Kanzaria HK (2019) Reducing emergency department length of stay. JAMA 321(14):1402–1403. https://doi.org/10.1001/jama.2018.21812
Jiang J, Upfill-Brown A, Dann AM et al (2019) Association of hospital length of stay and complications with readmission after open pancreaticoduodenectomy. JAMA Surg 154(1):88–90. https://doi.org/10.1001/jamasurg.2018.3213
Adogwa O, Lilly DT, Khalid S et al (2019) Extended length of stay after lumbar spine surgery: sick patients, postoperative complications, or practice style differences among hospitals and physicians? World Neurosurg 123:e734–e739. https://doi.org/10.1016/j.wneu.2018.12.016
Gay JC, Hall M, Markham JL, Bettenhausen JL, Doupnik SK, Berry JG (2019) Association of extending hospital length of stay with reduced pediatric hospital readmissions. JAMA Pediatr 173(2):186–188. https://doi.org/10.1001/jamapediatrics.2018.3815
Sahni NR, Carrus B, Cutler DM (2021) Administrative simplification and the potential for saving a quarter-trillion dollars in health care. JAMA 326(17):1677–1678. https://doi.org/10.1001/jama.2021.17315
Blackburn CW, Thompson NR, Tanenbaum JE, Passerallo AJ, Mroz TE, Steinmetz MP (2019) Association of cost savings and surgical quality with single-vendor procurement for spinal implants. JAMA Netw Open 2(11):e1915567. https://doi.org/10.1001/jamanetworkopen.2019.15567
Peterson KA, Zehri AH, Lee KE et al (2021) Current trends in incidence, characteristics, and surgical management of metastatic breast cancer to the spine: a National Inpatient Sample analysis from 2005 to 2014. J Clin Neurosci 91:99–104. https://doi.org/10.1016/j.jocn.2021.06.043
de Carvalho Almeida RF, Serra HO, de Oliveira LP (2021) Fast-track versus conventional surgery in relation to time of hospital discharge following total hip arthroplasty: a single-center prospective study. J Orthop Surg Res 16(1):488. https://doi.org/10.1186/s13018-021-02640-x
Wang KY, Puvanesarajah V, Xu A et al (2022) Growing racial disparities in the utilization of adult spinal deformity surgery: an analysis of trends from 2004 to 2014. Spine (Phila Pa 1976) 47(7):E283–E289. https://doi.org/10.1097/BRS.0000000000004180
Robinson S (2012) Neonatal posthemorrhagic hydrocephalus from prematurity: pathophysiology and current treatment concepts: a review. J Neurosurg Pediatr 9(3):242–258
Pieper CH, Smith J, Maree D, Pohl FC (2003) Is nCPAP of value in extreme preterms with no access to neonatal intensive care? J Trop Pediatr 49(3):148–152. https://doi.org/10.1093/tropej/49.3.148
Bolisetty S, Dhawan A, Abdel-Latif M et al (2014) Intraventricular hemorrhage and neurodevelopmental outcomes in extreme preterm infants. Pediatrics 133(1):55–62. https://doi.org/10.1542/peds.2013-0372
Lechtholz-Zey E, Bonney PA, Cardinal T et al (2022) Systematic review of racial, socioeconomic, and insurance status disparities in the treatment of pediatric neurosurgical diseases in the United States. World Neurosurg 158:65–83
Maddy K, Eliahu K, Bryant J-P et al (2023) Healthcare disparities in pediatric neurosurgery: a scoping review. J Neurosurg Pediatr 1(aop):1–12
Murosko D, Passerella M, Lorch S (2020) Racial segregation and intraventricular hemorrhage in preterm infants. Pediatr. https://doi.org/10.1542/peds.2019-1508
Shankaran S, Lin A, Maller-Kesselman J et al (2014) Maternal race, demography, and health care disparities impact risk for intraventricular hemorrhage in preterm neonates. J Pediatr 164(5):1005–1011. https://doi.org/10.1016/j.jpeds.2014.01.036
Ballabh P (2010) Intraventricular hemorrhage in premature infants: mechanism of disease. Pediatr Res 67(1):1–8. https://doi.org/10.1203/PDR.0b013e3181c1b176
Basiri B, Sabzehei MK, ShokouhiSolgi M, Khanlarzadeh E, Mosheiri M (2021) The frequency of intraventricular hemorrhage and its risk factors in premature neonates in a hospitalʼs NICU. Iran J Child Neurol Summer 15(3):109–118. https://doi.org/10.22037/ijcn.v15i3.21592
Philip AG, Allan WC, Tito AM, Wheeler LR (1989) Intraventricular hemorrhage in preterm infants: declining incidence in the 1980s. Pediatrics 84(5):797–801
Wilson-Costello D, Friedman H, Minich N, Fanaroff AA, Hack M (2005) Improved survival rates with increased neurodevelopmental disability for extremely low birth weight infants in the 1990s. Pediatrics 115(4):997–1003. https://doi.org/10.1542/peds.2004-0221
Vohr BR, Allan WC, Westerveld M et al (2003) School-age outcomes of very low birth weight infants in the indomethacin intraventricular hemorrhage prevention trial. Pediatrics 111(4 Pt 1):e340–e346. https://doi.org/10.1542/peds.111.4.e340
Kahle KT, Kulkarni AV, Limbrick DD Jr, Warf BC (2016) Hydrocephalus in children. Lancet 387(10020):788–799. https://doi.org/10.1016/S0140-6736(15)60694-8
Kulkarni AV, Riva-Cambrin J, Butler J et al (2013) Outcomes of CSF shunting in children: comparison of Hydrocephalus Clinical Research Network cohort with historical controls: clinical article. J Neurosurg Pediatr 12(4):334–338. https://doi.org/10.3171/2013.7.PEDS12637
Karimy JK, Reeves BC, Damisah E et al (2020) Inflammation in acquired hydrocephalus: pathogenic mechanisms and therapeutic targets. Nat Rev Neurol 16(5):285–296. https://doi.org/10.1038/s41582-020-0321-y
Christian EA, Jin DL, Attenello F et al (2016) Trends in hospitalization of preterm infants with intraventricular hemorrhage and hydrocephalus in the United States, 2000–2010. J Neurosurg Pediatr 17(3):260–269. https://doi.org/10.3171/2015.7.PEDS15140
Blum JD, Ng JJ, Craig J et al (2023) Sociodemographic disparities in craniosynostosis: a systematic review. Cleft Palate Craniofac J 0(0). https://doi.org/10.1177/10556656231199832
Hoffman C, Valenti AB, Odigie E, Warren K, Premaratne ID, Imahiyerobo TA (2021) Impact of health disparities on treatment for single-suture craniosynostosis in an era of multimodal care. Neurosurg Focus 50(4):E13
Travers CP, Carlo WA, McDonald SA et al (2020) Racial/ethnic disparities among extremely preterm infants in the United States from 2002 to 2016. JAMA Netw Open 3(6):e206757–e206757
Humberg A, Härtel C, Paul P et al (2017) Delivery mode and intraventricular hemorrhage risk in very-low-birth-weight infants: observational data of the German Neonatal Network. Eur J Obstet Gynecol Reprod Biol 212:144–149
Fortmann I, Mertens L, Boeckel H et al (2022) A timely administration of antenatal steroids is highly protective against intraventricular hemorrhage: an observational multicenter cohort study of very low birth weight infants. Front Pediatr 10:721355
Howell EA, Janevic T, Hebert PL, Egorova NN, Balbierz A, Zeitlin J (2018) Differences in morbidity and mortality rates in black, white, and Hispanic very preterm infants among New York City hospitals. JAMA Pediatr 172(3):269–277
Hebert PL, Chassin MR, Howell EA (2011) The contribution of geography to black white differences in the use of low neonatal mortality hospitals in New York City. Med Care 49(2):200–206. https://doi.org/10.1097/MLR.0b013e3182019144
Profit J, Gould JB, Bennett M et al (2017) Racial/ethnic disparity in NICU quality of care delivery. Pediatrics 140(3). https://doi.org/10.1542/peds.2017-0918
Author information
Authors and Affiliations
Contributions
Sumaiya Sayeed, B.S: software, methodology, formal analysis, writing — original draft; Benjamin C. Reeves, B.A.: writing — original draft; Brianna C. Theriault, M.D., Ph.D.: writing — original draft; Astrid C. Hengartner, B.S.: writing — review and editing; Nabihah Ahsan: writing — original draft; Sina Sadeghzadeh, A.B.: writing — Review and editing; Emad A. Elsamadicy, M.D., M.S.: writing — review and editing, supervision; Michael DiLuna, M.D.: writing — review and editing, supervision; Aladine A. Elsamadicy, M.D.: conceptualization, writing — review and editing, supervision.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sayeed, S., Reeves, B.C., Theriault, B.C. et al. Reduced racial disparities among newborns with intraventricular hemorrhage. Childs Nerv Syst (2024). https://doi.org/10.1007/s00381-024-06369-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00381-024-06369-w