Abstract
Purpose
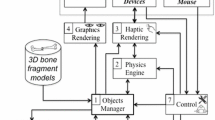
Untethering surgery for lumbosacral lipoma is a preventive procedure, and avoidance of complications and good long-term outcomes are required. We introduced presurgical interactive virtual simulation (IVS) applying three-dimensional multifusion images using a haptic device aimed at improving operative outcomes.
Methods
Fourteen patients with newly diagnosed lumbosacral lipoma were recruited and underwent preoperative IVS. The median age at surgery was 8 months. A three-dimensional image analysis system was used to extract and fuse structures necessary for surgery, such as the lipoma, spinal cord and skin, from CT and MRI, and create three-dimensional multifusion images. The created images were individually converted to standard triangulated language format and loaded onto a workstation (Geomagic freeform™) that could be freely transformed, and the laminectomy range and lipoma extraction procedure were examined. Presurgical IVS was performed, and the actual surgery was performed.
Results
The disease types were dorsal, caudal, lipomyelomeningocele, transitional, and filum in 5, 5, 2, 1, and 1 patients, respectively. The surgical procedure and extent of the laminectomy were as planned for all patients. Resection of the lipomas tended to be less than expected preoperatively because of positive reactions on intraoperative monitoring. No postoperative complications were observed. The median postoperative follow-up period was 29 months, and there were no reoperations during the observation period.
Conclusions
Although there are various types of lumbosacral lipoma, surgery can be safely performed by performing presurgical IVS. The short-term course is good; however, long-term follow-up is necessary for the appearance of neurological symptoms associated with growth and re-tethering.



Similar content being viewed by others
References
Oishi M, Fukuda M, Hiraishi T, Yajima N, Sato Y, Fujii Y (2012) Interactive virtual simulation using a 3D computer graphics model for microvascular decompression Surgery. J Neurosurg 117(3):555–565. https://doi.org/10.3171/2012.5.JNS112334
Hiraishi T, Matsushima T, Kawashima M et al (2013) 3D computer graphics simulation to obtain optimal surgical exposure during microvascular decompression of the glossopharyngeal nerve. Neurosurg Rev 36(4):629–635. https://doi.org/10.1007/s10143-013-0479-5
Seto H, Ogura R, Hiraishi T et al (2023) Preoperative three-dimensional multifusion imaging aiding successful microvascular decompression of a cerebellopontine angle lipoma: associated hemifacial spasm. Illustrative case. J Neurosurg Case Lessons. ;5(12):CASE2318. Published 2023 Mar 20. https://doi.org/10.3171/CASE2318
Harada A, Nishiyama K, Yoshimura J, Sano M, Fujii Y (2014) Intraspinal lesions associated with sacrococcygeal dimples. J Neurosurg Pediatr 14(1):81–86. https://doi.org/10.3171/2014.4.PEDS13431
Ogura R, Oishi M, Hiraishi T et al (2021) Four-dimensional multifusion imaging for assessment of meningioma hemodynamics. Interdiscip Neurosurg 24:101118
Pang D (2015) Total resection of Complex spinal cord Lipomas: how, why, and when to operate? Neurol Med Chir (Tokyo) 55(9):695–721. https://doi.org/10.2176/nmc.ra.2014-0442
Hoffman HJ, Hendrick EB, Humphreys RP (1976) The tethered spinal cord: its protean manifestations, diagnosis and surgical correction. Childs Brain 2(3):145–155. https://doi.org/10.1159/000119610
Hoffman HJ, Taecholarn C, Hendrick EB, Humphreys RP (1985) Management of lipomyelomeningoceles. Experience at the hospital for Sick Children, Toronto. J Neurosurg 62(1):1–8. https://doi.org/10.3171/jns.1985.62.1.0001
Finn MA, Walker ML (2007) Spinal lipomas: clinical spectrum, embryology, and treatment. Neurosurg Focus 23(2):E10. https://doi.org/10.3171/FOC-07/08/E10
Blount JP, Elton S (2001) Spinal lipomas. Neurosurg Focus. ;10(1):e3. Published 2001 Jan 15. https://doi.org/10.3171/foc.2001.10.1.4
Arai H, Sato K, Okuda O et al (2001) Surgical experience of 120 patients with lumbosacral lipomas. Acta Neurochir (Wien) 143(9):857–864. https://doi.org/10.1007/s007010170015
Oi S, Nomura S, Nagasaka M et al (2009) Embryopathogenetic surgicoanatomical classification of dysraphism and surgical outcome of spinal lipoma: a nationwide multicenter cooperative study in Japan. J Neurosurg Pediatr 3(5):412–419. https://doi.org/10.3171/2009.1.PEDS08168
Morota N, Ihara S, Ogiwara H (2017) New classification of spinal lipomas based on embryonic stage. J Neurosurg Pediatr 19(4):428–439. https://doi.org/10.3171/2016.10.PEDS16247
Hashiguchi K, Morioka T, Fukui K et al (2005) Usefulness of constructive interference in steady-state magnetic resonance imaging in the presurgical examination for lumbosacral lipoma. J Neurosurg 103(6 Suppl):537–543. https://doi.org/10.3171/ped.2005.103.6.0537
Udupa JK, Hung HM, Chuang KS (1991) Surface and volume rendering in three-dimensional imaging: a comparison. J Digit Imaging 4(3):159–168. https://doi.org/10.1007/BF03168161
Bamba Y, Nonaka M, Nakajima S, Yamasaki M (2011) Three-dimensional reconstructed computed tomography-magnetic resonance fusion image-based preoperative planning for surgical procedures for spinal lipoma or tethered spinal cord after myelomeningocele repair. Neurol Med Chir (Tokyo) 51(5):397–402. https://doi.org/10.2176/nmc.51.397
Oishi M, Fukuda M, Yajima N et al (2013) Interactive presurgical simulation applying advanced 3D imaging and modeling techniques for skull base and deep tumors. J Neurosurg 119(1):94–105. https://doi.org/10.3171/2013.3.JNS121109
Ogawa Y, Hayashi H, Sasaki R et al (2023) Motor-evoked potential monitoring from urinary sphincter muscle during pediatric untethering Surgery: a case series [published online ahead of print, 2023 Mar 9]. Childs Nerv Syst. https://doi.org/10.1007/s00381-023-05895-3
Nonaka M, Itakura T, Iwamura H et al (2023) Comparison of intraoperative neurophysiological monitoring methods for lumbosacral lipoma Surgery in infants. Childs Nerv Syst 39(6):1603–1610. https://doi.org/10.1007/s00381-023-05900-9
Byrne RW, Hayes EA, George TM, McLone DG (1995) Operative resection of 100 spinal lipomas in infants less than 1 year of age. Pediatr Neurosurg 23(4):182–187. https://doi.org/10.1159/000120956
Xenos C, Sgouros S, Walsh R, Hockley A (2000) Spinal lipomas in children. Pediatr Neurosurg 32(6):295–307. https://doi.org/10.1159/000028958
Pang D, Zovickian J, Oviedo A (2010) Long-term outcome of total and near-total resection of spinal cord lipomas and radical reconstruction of the neural placode, part II: outcome analysis and preoperative profiling. Neurosurgery 66(2):253–273. https://doi.org/10.1227/01.NEU.0000363598.81101.7B
Acknowledgements
The authors thank Yoshiyuki Noto, Tatsuya Kuramoto and Hiroaki Saito, Department of Radiological Technology, Niigata University Hospital, for their technical assistance.
Author information
Authors and Affiliations
Contributions
R.O. and M.O. conceived the idea of the study. R.O. and M.N. wrote the main manuscript text and prepared Figs. 1, 2 and 3. F.H., T.H. and M.S. contributed to the interpretation of the results. M.O. supervised the conduct of this study. All authors critically reviewed and revised the manuscript draft and approved the final version for submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ogura, R., Fujiwara, H., Natsumeda, M. et al. Preoperative interactive virtual simulation applying three-dimensional multifusion images using a haptic device for lumbosacral lipoma. Childs Nerv Syst 40, 1129–1136 (2024). https://doi.org/10.1007/s00381-023-06234-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-023-06234-2