Abstract
Introduction
Craniopharyngioma constitutes approximately 10% of primary brain tumors in children. It can cause considerable morbidity and mortality due to the local aggressiveness of the tumor itself or its management affecting the hypothalamus-pituitary axis and optic pathway involvement. There is very scarce data available from LMIC which makes the management controversial where multidisciplinary teams are already not available in most of the centers. This is a single-center cross-sectional retrospective review of 20-year record of 49 patients with craniopharyngioma treated between 2001 and 2020 at Aga Khan University Hospital, a tertiary care center in Karachi, Pakistan.
Methods
We have assessed the epidemiological data of children presenting with the diagnosis of craniopharyngioma, treatment modalities used, and neurological, endocrine, and hypothalamic complications in these patients. The assessment involved a retrospective review of medical records and medical follow-up.
Results
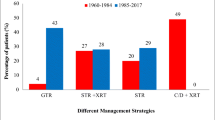
Out of a total of 49 patients, 26 (53%) were male, and 23 (46.9%) were female. The mean age was 9.5 years (SD ± 4.5 years). Most common symptoms at initial presentation were headache 41 (83.6%), visual deficit 40 (81.6%), nausea and vomiting 26 (53%), and endocrine abnormalities 16 (32%). Treatment modalities used at our center include gross total resection 11 (22%) and subtotal resection 38 (77%) out of total, while 6 (12.2%) patients received intracystic interferon. Histopathologic findings of the majority of patients (40 (81%)) revealed an adamantinomatous type of tumor. Only 23 (46.9%) children followed in clinic post-op. Median follow-up after craniopharyngioma presentation was 5 years (± 2.1 SD, range: 2–10 years). Pituitary hormone deficiencies (98%) and visual disturbances (75%) were the most common long-term health conditions observed.
Conclusions
Since pituitary hormone deficiencies and visual disturbance were the most common long-term health conditions observed in our study, these patients require a multidisciplinary team follow-up to improve their quality of life.
Similar content being viewed by others
Abbreviations
- STR:
-
Subtotal resection
- GTR:
-
Gross total resection
- LMIC:
-
Low- or middle-income country
- BMI:
-
Body mass index
References
Hoffman HJ (1994) Surgical management of craniopharyngioma. Pediatr Neurosurg 21(Suppl. 1):44–49
Muller HL (2008) Childhood craniopharyngioma. Recent advances in diagnosis, treatment, and follow-up. Hormone Res 69(4):193–202
Müller HL (2010) Childhood craniopharyngioma—current concepts in diagnosis, therapy, and follow-up. Nat Rev Endocrinol 6(11):609–618
Poretti A, Grotzer MA, Ribi K, Schönle E, Boltshauser E (2004) Outcome of craniopharyngioma in children: long-term complications and quality of life. Dev Med Child Neurol 46(4):220–229
Fischer EG, Welch K, Shillito J, Winston KR, Tarbell NJ (1990) Craniopharyngiomas in children: long-term effects of conservative surgical procedures combined with radiation therapy. J Neurosurg 73(4):534–540
Grewal MR, Spielman DB, Safi C, Overdevest JB, Otten M, Bruce J et al (2020) Gross total versus subtotal surgical resection in the management of craniopharyngiomas. Allergy Rhinol 11:2152656720964158
Hoffman HJ, Hendrick EB, Humphreys RP, Buncic JR, Armstrong DL, Jenkin RD (1977) Management of craniopharyngioma in children. J Neurosurg 47(2):218–227
Haroon S, Afzal A, Zia S, Ali SJ, Zia F, Shamail F et al (2021) Clinicopathological features of craniopharyngioma: a 15-year study from a tertiary care center in Pakistan. Cureus 13(3):e14153. https://doi.org/10.7759/cureus.14153
Khalid MU, Shah MM, Bajwa MH, Mirza FA, Laghari AA (2022) Craniopharyngioma: a lower-middle-income-country epidemiology perspective. J Pak Med Assoc 72(Suppl 4)(11):S61–S67
Mazher S, Ashraf J (2015) Craniopharyngioma total or near total surgical resection: an outcome-based learning experience. Pak J Med Dent 4(01):10
Drapeau A, Walz PC, Eide JG, Rugino AJ, Shaikhouni A, Mohyeldin A et al (2019) Pediatric craniopharyngioma. Child’s Nervous. System 35:2133–2145
Lithgow K, Hamblin R, Pohl U, Karavitaki N (2022) Craniopharyngiomas. Endotext. http://www.endotext.org/
Hoffmann A, Boekhoff S, Gebhardt U, Sterkenburg AS, Daubenbüchel AM, Eveslage M et al (2015) History before diagnosis in childhood craniopharyngioma: associations with initial presentation and long-term prognosis. Eur J Endocrinol 173(6):853–862
Hoffman HJ, De Silva M, Humphreys RP, Drake JM, Smith ML, Blaser SI (1992) Aggressive surgical management of craniopharyngiomas in children. J Neurosurg 76(1):47–52
Müller H, Gebhardt U, Maroske J, Hanisch E (2011) Long-term follow-up of morbidly obese patients with childhood craniopharyngioma after laparoscopic adjustable gastric banding (LAGB). Klin Padiatr 223(06):372–373
Yaşargil MG, Curcic M, Kis M, Siegenthaler G, Teddy PJ, Roth P (1990) Total removal of craniopharyngiomas: approaches and long-term results in 144 patients. J Neurosurg 73(1):3–11
Abrams LS, Repka MX (1997) Visual outcome of craniopharyngioma in children. J Pediatr Ophthalmol Strabismus 34(4):223–228
Mortini P, Losa M, Pozzobon G, Barzaghi R, Riva M, Acerno S et al (2011) Neurosurgical treatment of craniopharyngioma in adults and children: early and long-term results in a large case series. J Neurosurg 114(5):1350–1359
Kumar S, Stecher G, Li M, Knyaz C, Tamura K (2018) MEGA X: molecular evolutionary genetics analysis across computing platforms. Mol Biol Evol 35(6):1547
DeVile CJ, Grant DB, Hayward RD, Stanhope R (1996) Growth and endocrine sequelae of craniopharyngioma. Arch Dis Child 75(2):108–114
Daneman D, Hoffman HJ, Ehrlich RM (1994) The endocrine outcome after surgical removal of craniopharyngiomas. Pediatr Neurosurg 21(1):24–27
Gonc EN, Yordam N, Ozon A, Alikasifoglu A, Kandemir N (2004) Endocrinological outcome of different treatment options in children with craniopharyngioma: a retrospective analysis of 66 cases. Pediatr Neurosurg 40(3):112–119
Karavitaki N, Brufani C, Warner J, Adams C, Richards P, Ansorge O et al (2005) Craniopharyngiomas in children and adults: systematic analysis of 121 cases with long-term follow-up. Clin Endocrinol 62(4):397–409
Stripp DC, Maity A, Janss AJ, Belasco JB, Tochner ZA, Goldwein JW et al (2004) Surgery with or without radiation therapy in the management of craniopharyngiomas in children and young adults. Int J Radiat Oncol Biol Phys 58(3):714–20
Webb KL, Pruter WW, Hinkle ML, Walsh MT (2023) Comparing surgical approaches for craniopharyngioma resection among adults and children: a meta-analysis and systematic review. World Neurosurg 175:e876–e896
Acknowledgements
No individuals other than the listed co-authors contributed to this publication.
Author information
Authors and Affiliations
Contributions
Dr Naureen Mushtaq and Dr Fozia Memon wrote the main manuscript text. Dr Khadija Nuzhat Humayun conceptualized the idea and did proofreading. Dr Kiran Hilal added the radiology section and reviewed the article. Dr Altaf Laghari and Dr Muzna Arif reviewed the article and did the final correction. All authors read and approved the final manuscript with corrections.
Corresponding author
Ethics declarations
Ethics approval
The retrospective data collection of this study has been approved by the institutional ethics committee (2022-7168-20979).
Consent for publication
All authors gave their consent for the publication.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Memon, F., Humayun, K.N., Riaz, Q. et al. Pediatric craniopharyngioma: a 20-year study on epidemiological features, clinical presentation, and survival outcomes in a tertiary care center from LMIC. Childs Nerv Syst 40, 427–434 (2024). https://doi.org/10.1007/s00381-023-06177-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-023-06177-8