Abstract
Purpose
Coccidioidal meningitis (CM) is an uncommon disease frequently misdiagnosed. Neuroimaging and mortality are not considered in detail in previous pediatric CM series. Our objective is to evaluate outcome of pediatric neurococcidiomycosis in relation to neuroimaging findings.
Methods
We performed a prospective, observational, cross-sectional study in children with hydrocephalus and CM treated at Specialties Hospital in Torreon, Mexico (between 2015 and 2020). The outcome was evaluated by Hydrocephalus Outcome Questionnaire (HOQ) and the modified Rankin Scale (mRS). Follow-up was established at the first shunt surgery and survival since CM diagnosis confirmation. Neuroimaging was analyzed in relation to clinical data, outcome and survival. Kaplan-Meier analysis was performed with IBM-SPSS-25.
Results
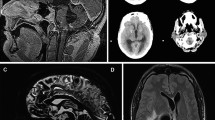
Ten pediatric cases with CM and hydrocephalus were reported. Aged 6–228 months, 60% were female. Mean number of surgeries was 4.3 SD ± 3 (range 1–15). Asymmetric hydrocephalus was the most common neuroimaging finding (70%), followed by cerebral vasculitis (20%) and isolated fourth ventricle (IFV) (20%). The mean HOQ overall score was 0.338 SD ± 0.35. A minimum follow-up of 18 months was reported. Mean survival was 13.9 SD ± 6.15 months (range 3–24). Poor survival was correlated with asymmetric hydrocephalus (p = 0.335), cerebral vasculitis (p = 0.176), IFV (p < 0.001), bacterial superinfection (p = 0.017), lower mRS scores at hospital discharge (p = 0.017) and during follow-up (p = 0.004). The mortality rate was 20%.
Conclusions
We report the largest series in Latin America of pediatric CM and hydrocephalus. Asymmetric hydrocephalus, IFV and cerebral vasculitis are complications that increase mortality and must be early diagnosed for a timely surgical and medical treatment. HOQ and mRS could be alternative scales to evaluate outcome in these patients. After a long follow-up (18 months), survival remained poor after diagnosis confirmation in our series.






Similar content being viewed by others
Availability of data material
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Hector RF, Laniado-Laborin R (2005) Coccidioidomycosis–a fungal disease of the Americas. PLoS Med 2:e2
McCotter OZ, Benedict K, Engelthaler DM, Komatsu K, Lucas KD, Mohle-Boetani JC, Oltean H, Vugia D, Chiller TM, Sondermeyer Cooksey GL, Nguyen A, Roe CC, Wheeler C, Sunenshine R (2019) Update on the epidemiology of coccidioidomycosis in the United States. Med Mycol 57:S30–S40
Odio CD, Marciano BE, Galgiani JN, Holland SM (2017) Risk factors for disseminated coccidioidomycosis, United States. Emerg Infect Dis 23
Gottfredsson M, Perfect JR (2000) Fungal meningitis. Semin Neurol 20:307–322
Bouza E, Dreyer JS, Hewitt WL, Meyer RD (1981) Coccidioidal meningitis. An analysis of thirty-one cases and review of the literature. Medicine (Baltimore) 60:139–172
Chiller TM, Galgiani JN, Stevens DA (2003) Coccidioidomycosis. Infect Dis Clin North Am 17: 41–57, viii
Johnson R, Ho J, Fowler P, Heidari A (2018) Coccidioidal meningitis: a review on diagnosis, treatment, and management of complications. Curr Neurol Neurosci Rep 18:19
Galgiani JN, Ampel NM, Blair JE, Catanzaro A, Geertsma F, Hoover SE, Johnson RH, Kusne S, Lisse J, MacDonald JD, Meyerson SL, Raksin PB, Siever J, Stevens DA, Sunenshine R, Theodore N (2016) 2016 Infectious Diseases Society of America (IDSA) clinical practice guideline for the treatment of coccidioidomycosis. Clin Infect Dis 63:e112-146
Harrison HR, Reynolds AF (1982) Trapped fourth ventricle in coccidioidal meningitis. Surg Neurol 17:197–199
Little AS, Zabramski JM, Nakaji P (2010) Simplified aqueductal stenting for isolated fourth ventricle using a small-caliber flexible endoscope in a patient with neurococcidiomycosis: technical case report. Neurosurgery 66:373–374; discussion 374
Crete RN, Gallmann W, Karis JP, Ross J (2018) Spinal Coccidioidomycosis: MR imaging findings in 41 patients. AJNR Am J Neuroradiol 39:2148–2153
Erly WK, Bellon RJ, Seeger JF, Carmody RF (1999) MR imaging of acute coccidioidal meningitis. AJNR Am J Neuroradiol 20:509–514
Lammering JC, Iv M, Gupta N, Pandit R, Patel MR (2013) Imaging spectrum of CNS coccidioidomycosis: prevalence and significance of concurrent brain and spinal disease. AJR Am J Roentgenol 200:1334–1346
Wrobel CJ, Meyer S, Johnson RH, Hesselink JR (1992) MR findings in acute and chronic coccidioidomycosis meningitis. AJNR Am J Neuroradiol 13:1241–1245
Drake KW, Adam RD (2009) Coccidioidal meningitis and brain abscesses: analysis of 71 cases at a referral center. Neurology 73:1780–1786
Cardenas G, Aristizabal S, Salinas C, Delgado-Hernandez R, Angeles-Morales V, Soto-Hernandez J, Castanon-Olivares LR, Hernandez F (2020) Coccidioidal meningitis in non-AIDS patients. A case series at a Mexican neurological referral center. Clin Neurol Neurosurg 196:106011
Naeem F, McCarty J, Mhaissen MN, Ha S, Rongkavilit C (2019) Extrapulmonary coccidioidomycosis among children in central California: a retrospective review. Pediatr Infect Dis J 38:1189–1194
Saitoh A, Homans J, Kovacs A (2000) Fluconazole treatment of coccidioidal meningitis in children: two case reports and a review of the literature. Pediatr Infect Dis J 19:1204–1208
McCarty JM, Demetral LC, Dabrowski L, Kahal AK, Bowser AM, Hahn JE (2013) Pediatric coccidioidomycosis in central California: a retrospective case series. Clin Infect Dis 56:1579–1585
Lee LA, Sondermeyer Cooksey GL, Kim JJ, Kahal A, Gilliss D, Naeem F, McCarty JM, Vugia DJ (2019) Pediatric coccidioidomycosis: case series from a California Pediatric Infectious Diseases Clinic. Pediatr Infect Dis J 38:115–121
Dimitrova D, Ross L (2016) Coccidioidomycosis: experience from a children’s hospital in an area of endemicity. J Pediatric Infect Dis Soc 5:89–92
De la Cerda-Vargas MF, Sandoval-Bonilla BA, McCarty JM, De Leon FC, Candelas-Rangel JA, Rodriguez-Rodriguez JD, Navarro-Dominguez P, Munoz-Hernandez MA, Meza-Mata E, Fernandez-Gonzalez EM, Samano-Avina MG (2021) Hydrocephalus in Mexican children with coccidioidal meningitis: clinical, serological, and neuroimaging findings. Surg Neurol Int 12:119
Arsura EL, Johnson R, Penrose J, Stewart K, Kilgore W, Reddy CM, Bobba RK (2005) Neuroimaging as a guide to predict outcomes for patients with coccidioidal meningitis. Clin Infect Dis 40:624–627
Shetter AG, Fischer DW, Flom RA (1985) Computed tomography in cases of coccidioidal meningitis, with clinical correlation. West J Med 142:782–786
Kulkarni AV, Rabin D, Drake JM (2004) An instrument to measure the health status in children with hydrocephalus: the Hydrocephalus Outcome Questionnaire. J Neurosurg 101:134–140
Iglesias S, Ros B, Martin A, Carrasco A, Rius F, Arraez MA (2018) Functional outcome in pediatric hydrocephalus: results of applying the Spanish version of the Hydrocephalus Outcome Questionnaire. J Neurosurg Pediatr 21:224–235
Kalita J, Misra UK, Dubey AK (2019) Role of oxidative stress in tuberculous meningitis: a clinico-radiological correlation. J Mol Neurosci 68:287–294
Davis AG, Nightingale S, Springer PE, Solomons R, Arenivas A, Wilkinson RJ, Anderson ST, Chow FC, Tuberculous Meningitis International Research C (2019) Neurocognitive and functional impairment in adult and paediatric tuberculous meningitis. Wellcome Open Res 4:178
Segev Y, Metser U, Beni-Adani L, Elran C, Reider G II, Constantini S (2001) Morphometric study of the midsagittal MR imaging plane in cases of hydrocephalus and atrophy and in normal brains. AJNR Am J Neuroradiol 22:1674–1679
Kumar R (1999) Unilateral hydrocephalus in paediatric patients, a trial of endoscopic fenestration. Neurol India 47:282–285
Alexander E Jr, Botterell EH (1949) Unilateral hydrocephalus resulting from occlusion of foramen of Monro; complication of radical removal of brain abscess. J Neurosurg 6:197–206
Boyar B, Ildan F, Bagdatoglu H, Cetinalp E, Karadayi A (1993) Unilateral hydrocephalus resulting from occlusion of foramen of Monro: a new procedure in the treatment: stereotactic fenestration of the septum pellucidum. Surg Neurol 39:110–114
Milhorat TH, Hammock MK, Breckbill DL (1975) Acute unilateral hydrocephalus resulting from oedematous occlusion of foramen of Monro: complication of intraventricular surgery. J Neurol Neurosurg Psychiatry 38:745–748
Tager D, Hatch A, Segar J, Roller B, Al Mohajer M, Zangeneh TT (2017) Coccidioidal meningitis complicated by central nervous system vasculitis in a patient with leukemia. Med Mycol Case Rep 16:8–11
Ali K, Nannapaneni R, Hamandi K (2013) The isolated fourth ventricle. BMJ Case Rep 2013
Vucicevic D, Blair JE, Binnicker MJ, McCullough AE, Kusne S, Vikram HR, Parish JM, Wengenack NL (2010) The utility of Coccidioides polymerase chain reaction testing in the clinical setting. Mycopathologia 170:345–351
Binnicker MJ, Popa AS, Catania J, Alexov M, Tsaras G, Lloyd F, Wengenack NL, Enzler MJ (2011) Meningeal coccidioidomycosis diagnosed by real-time polymerase chain reaction analysis of cerebrospinal fluid. Mycopathologia 171:285–289
Kassis C, Zaidi S, Kuberski T, Moran A, Gonzalez O, Hussain S, Hartmann-Manrique C, Al-Jashaami L, Chebbo A, Myers RA, Wheat LJ (2015) Role of Coccidioides antigen testing in the cerebrospinal fluid for the diagnosis of coccidioidal meningitis. Clin Infect Dis 61:1521–1526
Engelmann KA, Jordan LC (2012) Outcome measures used in pediatric stroke studies: a systematic review. Arch Neurol 69:23–27
Kulkarni AV, Drake JM, Rabin D, Dirks PB, Humphreys RP, Rutka JT (2004) Measuring the health status of children with hydrocephalus by using a new outcome measure. J Neurosurg 101:141–146
Platenkamp M, Hanlo PW, Fischer K, Gooskens RH (2007) Outcome in pediatric hydrocephalus: a comparison between previously used outcome measures and the Hydrocephalus Outcome Questionnaire. J Neurosurg 107:26–31
Mischel PS, Vinters HV (1995) Coccidioidomycosis of the central nervous system: neuropathological and vasculopathic manifestations and clinical correlates. Clin Infect Dis 20:400–405
Shehab ZM, Britton H, Dunn JH (1988) Imidazole therapy of coccidioidal meningitis in children. Pediatr Infect Dis J 7:40–44
Levy ER, McCarty JM, Shane AL, Weintrub PS (2013) Treatment of pediatric refractory coccidioidomycosis with combination voriconazole and caspofungin: a retrospective case series. Clin Infect Dis 56:1573–1578
Romeo JH, Rice LB, McQuarrie IG (2000) Hydrocephalus in coccidioidal meningitis: case report and review of the literature. Neurosurgery 47:773–777
Johnson RH, Einstein HE (2006) Coccidioidal meningitis. Clin Infect Dis 42:103–107
Vincent T, Galgiani JN, Huppert M, Salkin D (1993) The natural history of coccidioidal meningitis: VA-Armed Forces cooperative studies, 1955–1958. Clin Infect Dis 16:247–254
Hardesty DA, Ramey W, Afrasiabi M, Beck B, Gonzalez O, Moran A, Nakaji P (2014) Patient outcomes and surgical complications in coccidioidomycosis-related hydrocephalus: an institutional review. J Neurosurg 121:785–789
Platenkamp M HP, Fischer K, Gooskens RH. Outcome in pediatric hydrocephalus: a comparison between previously used outcome measures and the Hydrocephalus Outcome Questionnaire. J Neurosurg 107: 26–31
Quinn TJ, Dawson J, Walters MR, Lees KR (2009) Reliability of the modified Rankin Scale: a systematic review. Stroke 40:3393–3395
Acknowledgements
We are grateful to Professor Abhaya V. Kulkarni for his advice on HOQ calculation. We express our acknowledgment to the National Council of Science and Technology (CONACyT) from Mexico.
Author information
Authors and Affiliations
Contributions
María F. De la Cerda-Vargas wrote the main manuscript. Author MF had the conception of the study and was in charge of data collection and analysis. B.A. Sandoval-Bonilla, José A. Candelas-Rangel and Pedro Navarro-Domínguez were in charge of writing the manuscript and editing the images, tables, and figures. B.A. Sandoval-Bonilla and Luis H. Ramirez-Silva wrote and edited the manuscript in English. Elizabeth Meza-Mata provided images and descriptions of pathological studies. Melisa A. Muñoz- Hernández and F. K. Segura-López performed the statistical analysis and review of the results of the study. Marisela Del Rocio González-Martínez, and Héctor A. Delgado-Aguirre supported the review of the literature and preparation of discussion and analysis. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the institutional research ethics committee (Local Health Research Committee 501, COFEPRIS 17 CI 05 035 078, Institutional registration ID R-2021-501-054). We certify that this study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. Children’s tutors signed informed consent before surgery, sampling for laboratory, and pathologic studies. No personally identifiable data or photographs of the participants are exposed in this study. Informed consent was not required because the information was anonymized and the submission does not include images that may identify the person. All children’s tutors signed informed consent to participate in the study (before surgery, sampling for laboratory and pathology, interviews (HOQ), etc.).
Consent for publication
Informed consent was obtained from legal guardians.
Conflict of interest
There are no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1
Appendix 2
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
De la Cerda-Vargas, M.F., Candelas-Rangel, J.A., Navarro-Dominguez, P. et al. Neurococcidiomycosis in children with hydrocephalus: assessment of functional outcome, quality of life and survival in relation to neuroimaging findings. Childs Nerv Syst 40, 303–319 (2024). https://doi.org/10.1007/s00381-023-06166-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-023-06166-x