Abstract
Purpose
We previously developed a novel functional benchtop apparatus to simulate catheter occlusion in vitro utilizing avian vitelline membrane and chalaza to test catheter designs and de-obstruction techniques. Here, we study the integration of double-lumen catheter-mediated backflow in the shunt system assembly and its potential for an in-line de-obstruction of an obstructed ventricular catheter.
Methods
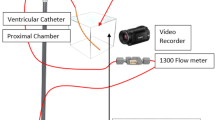
A double-lumen catheter was connected to a standard proximal shunt catheter for all trials. One limb of the double-lumen catheter was connected to the backflow mechanisms and allowed to loop back for fluid access. A micropump and a bi-corporal electromagnetic pump were utilized to provide various degrees of backflow at predetermined intervals. Flow rates were measured after initial occlusion and after implementation of the backflow mechanisms, and degrees of catheter blockage was calculated as a percentage of the unoccluded flow rate. Flow visualization was also used.
Results
In baseline blockage of less than 50%, the average occluding agent weighed 0.3–0.6 g with baseline flow rates of 8.5–11.9 mL/min. After 5 min of backflow using a micropump, the degree of blockage was reduced in 50% of trials. Additional backflow for 5 min did not provide further improvements in flow rate. In baseline blockage of greater than 50%, the average occluding agent weighed 0.8–1.3 g with baseline flow rates of 1.1–4.2 mL/min. After 5 min of backflow, the system demonstrated a decreased blockage in 20% of trials; additional backflow for 5 min further improved the flow rate in 40% of the total trials. Only magnetic plates provided enough force to provide pulsatile backflow in the bi-corporal electromagnetic system.
Conclusions
The preliminary results of connecting a standard proximal catheter in series with a double-lumen catheter show a slight change in the percent occlusion from the baseline status several times when the retrograde flow occurred via one limb of the catheter. Additionally, the de-obstruction seems related to the length of the interval of the backflow and the initial percentage occlusion of the proximal catheter. The statistical analysis does not reveal a statistically significant reduction in occlusion in the proximal catheter with either backflow interval.







Similar content being viewed by others
References
Kahle KT, Kulkarni AV, Limbrick DD Jr, Warf BC (2016) Hydrocephalus in children. Lancet (London, England) 387(10020):788–799. https://doi.org/10.1016/S0140-6736(15)60694-8
Weisenberg SH, TerMaath SC, Seaver CE, Killeffer JA (2016) Ventricular catheter development: past, present, and future. J Neurosurg 125(6):1504–1512. https://doi.org/10.3171/2015.12.JNS151181
Piatt JH Jr, Cosgriff M (2007) Monte Carlo simulation of cerebrospinal fluid shunt failure and definition of instability among shunt-treated patients with hydrocephalus. J Neurosurg 107(6 Suppl):474–478. https://doi.org/10.3171/PED-07/12/474
Sainte-Rose C, Piatt JH, Renier D, Pierre-Kahn A, Hirsch JF, Hoffman HJ, Humphreys RP, Hendrick EB (1991) Mechanical complications in shunts. Pedia Neurosurg 17(1):2–9. https://doi.org/10.1159/000120557
Go KG, Ebels EJ, van Woerden H (1981) Experiences with recurring ventricular catheter obstructions. Clin Neurol Neurosurg 83(2):47–56. https://doi.org/10.1016/0303-8467(81)90001-9
Kestle J, Drake J, Milner R, Sainte-Rose C, Cinalli G, Boop F, Piatt J, Haines S, Schiff S, Cochrane D, Steinbok P, MacNeil N (2000) Long-term follow-up data from the shunt design trial. Pedia Neurosurg 33(5):230–236. https://doi.org/10.1159/000055960
Zemack G, Romner B (2000) Seven years of clinical experience with the programmable Codman Hakim valve: a retrospective study of 583 patients. J Neurosurg 92(6):941–948. https://doi.org/10.3171/jns.2000.92.6.0941
Borgbjerg BM, Gjerris F, Albeck MJ, Hauerberg J, Børgesen SE (1995) Frequency and causes of shunt revisions in different cerebrospinal fluid shunt types. Acta Neurochir 136(3–4):189–194. https://doi.org/10.1007/BF01410625
Stone JJ, Walker CT, Jacobson M, Phillips V, Silberstein HJ (2013) Revision rate of pediatric ventriculoperitoneal shunts after 15 years. J Neurosurg Pediatr 11(1):15–19. https://doi.org/10.3171/2012.9.PEDS1298
Galarza M, Etus V, Sosa F, Argañaraz R, Mantese B, Gazzeri R, Montoya CG, de la Rosa P, Guerrero AL, Chaban G, Giménez Á, Amigó JM (2021) Flow ventricular catheters for shunted hydrocephalus: initial clinical results. Childs Nerv Syst 37(3):903–911. https://doi.org/10.1007/s00381-020-04941-8
Galarza M, Giménez A, Amigó JM, Schuhmann M, Gazzeri R, Thomale U, McAllister JP 2nd (2018) Next generation of ventricular catheters for hydrocephalus based on parametric designs. Childs Nerv Syst 34(2):267–276. https://doi.org/10.1007/s00381-017-3565-0
Galarza M, Giménez Á, Valero J, Pellicer OP, Amigó JM (2014) Computational fluid dynamics of ventricular catheters used for the treatment of hydrocephalus: a 3D analysis. Childs Nerv Syst 30(1):105–116. https://doi.org/10.1007/s00381-013-2226-1
Giménez Á, Galarza M, Pellicer O, Valero J, Amigó JM (2016) Influence of the hole geometry on the flow distribution in ventricular catheters for hydrocephalus. Biomed Eng Online 15 Suppl 1;71. https://doi.org/10.1186/s12938-016-0182-1
Harris CA, McAllister JP 2nd (2011) Does drainage hole size influence adhesion on ventricular catheters? Childs Nerv Syst 27(8):1221–1232. https://doi.org/10.1007/s00381-011-1430-0
Lin J, Morris M, Olivero W, Boop F, Sanford RA (2003) Computational and experimental study of proximal flow in ventricular catheters. Technical note. J Neurosurg 99(2):426–431. https://doi.org/10.3171/jns.2003.99.2.0426
Qi D, Olson E, Ivankovic S, Sommer T, Nair K, Morris M, Lin J (2022) High-resistance proximal “scaled” ventricular catheters. Childs Nerv Syst 38(2):333–341. https://doi.org/10.1007/s00381-021-05390-7
Thomale UW, Hosch H, Koch A, Schulz M, Stoltenburg G, Haberl EJ, Sprung C (2010) Perforation holes in ventricular catheters–is less more? Childs Nerv Syst 26(6):781–789. https://doi.org/10.1007/s00381-009-1055-8
Qi D, Patel A, Dunwoody R, McCall S, Bach S, Lin J (2022) Proximal ventricular shunt catheter occlusion model. Childs Nerv Syst. Advance online publication. https://doi.org/10.1007/s00381-022-05689-z
Falcone J, Ho C, Eskandari R et al (2020) A noninvasive retrograde flushing system for shunted hydrocephalus: initial case series of 25 patients. Cureus 12(7):e8940. https://doi.org/10.7759/cureus.8940.
Acknowledgements
Previously presented at the 51st Annual Meeting of the AANS/CNS Section on Pediatric Neurological Surgery; December 01-04, 2022; Washington D.C.
Author information
Authors and Affiliations
Contributions
Anup Patel and Julian Lin wrote the main manuscript. Jacqueline Boyle edited the manuscript. Martin Morris supervised the engineering aspects and acquisition of data.
Corresponding author
Ethics declarations
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (MOV 32706 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Patel, A., Qi, D., Boyle, J. et al. Dual catheter and double-lumen cerebrospinal fluid shunt systems with backflow mechanisms. Childs Nerv Syst 40, 135–143 (2024). https://doi.org/10.1007/s00381-023-06101-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-023-06101-0