Abstract
Purpose
Neural tube defects (NTDs) are one of the most common congenital anomalies and a cause of chronic disability. The study was done to study outcomes of neural tube defects admitted at a tertiary level neonatal intensive care unit (NICU) from 2018 to 2022, a period of 4 years that also coincided with the COVID pandemic. The secondary outcome was to study the clinical presentation, associated anomalies and epidemiological features.
Methods
It was a retrospective observational study; data of infants was obtained from medical records and analysis was done.
Results
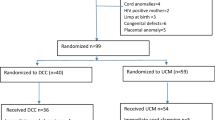
Thirty-four neonates were enrolled, of which there were 16 (47%) males and 18 (53%) females. History of pre-pregnancy maternal folate intake was present in 4 (11.7%) cases. 33 (97%) babies were diagnosed with meningomyelocele (MMC) and one each had anencephaly, iniencephaly and encephalocele, of which one had frontal and two had occipital encephalocele. The median age of surgery was 16 days of life with primary repair being the most common procedure followed by MMC repair with VP shunt. Twenty babies (58.8%) were discharged successfully, while 9 (26.5%) expired and 5 (14.7%) were discharged against medical advice; which can be attributed to the financial problems of the patients in a developing country. The overall deaths in our series were four (26.5%) which is slightly higher than other studies which may be due to the fact that this study was conducted during the COVID era with lesser rates of folate supplementation, reduced access to prenatal diagnosis coupled with poor follow-up and compliance of patients post-surgical repair.
Conclusion
This study emphasizes the importance of periconceptional folic acid supplementation, prenatal diagnosis, early surgery and meticulous follow-up as being pivotal to improving outcomes in children with NTDs.



Similar content being viewed by others
Abbreviations
- CSF:
-
Cerebrospinal Fluid
- EVD:
-
External ventricular device
- MMC:
-
Meningomyelocele
- NTDs:
-
Neural tube defects
- NICU:
-
Neonatal intensive care unit
- VP Shunt:
-
Ventriculoperitoneal shunt
- TIFFA:
-
Targeted imaging for fetal anomalies
References
Dubowitz V (1998) Closed spinal dysraphism. Eur J Paediatr Neurol 2(6):324–326. https://doi.org/10.1016/s1090-3798(98)80009-3. PMID: 10727201
Müller F, O’Rahilly R (1987) The development of the human brain, the closure of the caudal neuropore, and the beginning of secondary neurulation at stage 12. Anat Embryol (Berl) 176(4):413–430. https://doi.org/10.1007/BF00310083. PMID: 3688450
Avagliano L, Massa V, George T, Qureshy S, Bulfamante G, Finnell R (2018) Overview on neural tube defects: From development to physical characteristics. Birth Defects Research 12:111. https://doi.org/10.1002/bdr2.1380. PMID: 30421543
Ybot-Gonzalez P, Copp AJ (1999) Bending of the neural plate during mouse spinal neurulation is independent of actin microfilaments. Dev Dyn 215(3):273–83. https://doi.org/10.1002/(SICI)1097-0177(199907)215:3<273::AID-AJA9>3.0.CO;2H. PMID: 10398537
Schoner K, Axt-Fliedner R, Bald R, Fritz B, Kohlhase J, Kohl T et al (2017) Fetal Pathology of Neural Tube Defects – An Overview of 68 Cases. Geburtshilfe Frauenheilkd 1(77):495–507. https://doi.org/10.1055/s-0043-103459. PMID: 28579621
Rai S, Singh R, Pandey S, Singh K, Shinde N, Rai S et al (2016) High incidence of neural tube defects in Northern part of India. Asian J Neurosurg 1:11. https://doi.org/10.4103/1793-5482.175628. PMID: 27695536
Deak KL, Siegel DG, George TM, Gregory S, Ashley-Koch A, Speer MC et al (2008) Further evidence for a maternal genetic effect and a sex-influenced effect contributing to risk for human neural tube defects. Birth Defects Res A 82(10):662–669. https://doi.org/10.1002/bdra.20511. PMID: 18937341
Moretti ME, Bar-Oz B, Fried S, Koren G (2005) Maternal Hyperthermia and the Risk for Neural Tube Defects in Offspring: Systematic Review and Meta-Analysis. Epidemiology 16(2). https://doi.org/10.1097/01.ede.0000152903.55579.15. PMID: 15703536
Wen SW, Walker M (2004) Risk of Fetal Exposure to Folic Acid Antagonists. J Obstet Gynaecol Can 26(5):475–479. https://doi.org/10.1016/s1701-2163(16)30658-2. PMID: 15151734
Hernández-Díaz S, Werler MM, Walker AM, Mitchell AA (2001) Neural Tube Defects in Relation to Use of Folic Acid Antagonists during Pregnancy. Am J Epidemiol 153(10):961–968 PMID: 11384952
Ornoy A (2006) Neuroteratogens in man: An overview with special emphasis on the teratogenicity of antiepileptic drugs in pregnancy. Reprod Toxicol 22(2):214–226. https://doi.org/10.1016/j.reprotox.2006.03.014. PMID: 16621443
Crider KS, Bailey LB, Berry RJ (2011) Folic acid food fortification—its history, effect, concerns, and future directions. Nutrients 3:370–384. https://doi.org/10.3390/nu3030370. Epub 2011 Mar 15 PMID: 22254102
Berry RJ, Li Z, Erickson JD, Li S, Moore CA, Wang H et al (1999) Prevention of neural-tube defects with folic acid in China. N Engl J Med 341:1485–1490. https://doi.org/10.1056/NEJM199911113412001. PMID:10559448
Bowman RM, McLone DG, Grant JA, Tomita T, Ito JA (2001) Spina Bifida Outcome: A 25-Year Prospective. Pediatr Neurosurg 34(3):114–120. https://doi.org/10.1159/000056005. PMID: 11359098
Tennant PW, Pearce MS, Bythell M, Rankin J (2010) 20-year survival of children born with congenital anomalies: a population-based study. Lancet 375(9715):649–656. https://doi.org/10.1016/S0140-6736(09)61922-X. PMID: 20092884
Protzenko T, Bellas A, Pousa MS, Protzenko M, Fontes JM, de Lima Silveira AM et al (2019) Reviewing the prognostic factors in myelomeningocele. Neurosurgical Focus FOC 47(4):E2. https://doi.org/10.3171/2019.7.FOCUS19462. PMID: 31574474
Mehta VA, Bettegowda C, Ahmadi SA, Berenberg P, Thomale UW, Haberl EJ et al (2010) Spinal cord tethering following myelomeningocele repair: Clinical article. J Neurosurg Pediatr 6(5):498–505. https://doi.org/10.3171/2010.8.PEDS09491. PMID: 21039176
Kahle KT, Kulkarni AV, Limbrick DD, Warf BC (2016) Hydrocephalus in children. Lancet 387(10020):788–799. https://doi.org/10.1016/S0140-6736(15)60694-8. PMID: 26256071
Blencowe H, Kancherla V, Moorthie S, Darlison MW, Modell B (2018) Estimates of global and regional prevalence of neural tube defects for 2015: a systematic analysis. Ann NY Acad Sci 1414(1):31–46. https://doi.org/10.1111/nyas.13548. Epub 2018 Jan 24 PMID: 29363759
World Health Organization (2015) Global health estimates (GHE)–Cause-specific mortality. [cited 2015 Apr 14]. Available from http://www.who.int/healthinfo/globalburdendisease/estimates/en/index1.html
Wald NJ, Morris JK, Blakemore C (2018) Public health failure in the prevention of neural tube defects: Time to abandon the tolerable upper intake level of folate. Public Health Rev 39:2. https://doi.org/10.1186/s40985-018-0079-6
Salih MA, Murshid WR, Seidahmed MZ (2014) Epidemiology, prenatal management, and prevention of neural tube defects. Saudi Med J 35 Suppl 1(Suppl 1):S15–28. PMID: 25551106
Gedefaw A, Teklu S, Tadesse BT (2018) Magnitude of Neural Tube Defects and Associated Risk Factors at Three Teaching Hospitals in Addis Ababa, Ethiopia. Biomed Res Int 11(2018):4829023. https://doi.org/10.1155/2018/4829023. PMID: 29713643
Singh BK, Maria A, Bandyopadhyay T, Choudhary SK (2021) Clinico-epidemiological profile and outcomes of babies with neural tube defects in a tertiary care center in Northern India. J Matern Fetal Neonatal Med. https://doi.org/10.1080/14767058.2021.1937102. PMID: 34121591
Rehman L, Shiekh M, Afzal A, Rizvi R (2020) Risk factors, presentation and outcome of meningomyelocele repair. Pak J Med Sci 36(3):422–425. https://doi.org/10.12669/pjms.36.3.1237. PMID: 32292446
Wilson RD; SOGC Genetics committee; Special contributor (2014) RETIRED: Prenatal screening, diagnosis, and pregnancy management of fetal neural tube defects. J Obstet Gynaecol Can 36(10):927–939. https://doi.org/10.1016/S1701-2163(15)30444-8. PMID: 25375307
Airede IK (1992) Neural tube defects in the middle belt of Nigeria. J Trop Pediatr 38(1):27–29. https://doi.org/10.1093/tropej/38.1.27. PMID: 1573689
Chand MB, Agrawal J, Bista P (2011) Anaesthetic challenges and management of myelomeningocele repair. Postgrad Med J NAMS 11(1):41–46
Van Allen MI, Boyle E, Thiessen P, McFadden D, Cochrane D, Chambers GK, Langlois S, Stathers P, Irwin B, Cairns E, MacLeod P, Delisle MF, Uh SH (2006) The impact of prenatal diagnosis on neural tube defect (NTD) pregnancy versus birth incidence in British Columbia. J Appl Genet 47(2):151–158. https://doi.org/10.1007/BF03194615. PMID: 16682757
Tarcan T, Onol FF, Ilker Y, Alpay H, SimSek F, Ozek M (2006) The timing of primary neurosurgical repair significantly affects neurogenic bladder prognosis in children with myelomeningocele. J Urol 176(3):1161–1165. https://doi.org/10.1016/j.juro.2006.06.036. PMID: 16952698
Oncel MY, Ozdemir R, Kahilogulları G, Yurttutan S, Erdeve O, Dilmen U (2012) The effect of surgery time on prognosis in newborns with meningomyelocele. J Korean Neurosurg Soc 51(6):359–362. https://doi.org/10.3340/jkns.2012.51.6.359. PMID: 22949965
Ntimbani J, Kelly A, Lekgwara P (2020) Myelomeningocele –a literature review. Interdiscip Neurosurg 19:100502
Marreiros H, Loff C, Calado E (2015) Who needs surgery for pediatric myelomeningocele? A retrospective study and literature review. J Spinal Cord Med 38(5):626–640. https://doi.org/10.1179/2045772314Y.0000000229. PMID: 25029586
Dupepe EB, Hopson B, Johnston JM, Rozzelle CJ, Jerry Oakes W, Blount JP et al (2016) Rate of shunt revision as a function of age in patients with shunted hydrocephalus due to myelomeningocele. Neurosurg Focus 41(5):E6. https://doi.org/10.3171/2016.8.FOCUS16257
Pinto FC, Matushita H, Furlan AL, Alho EJ, Goldenberg DC, Bunduki V et al (2009) Surgical treatment of myelomeningocele carried out at ‘time zero’ immediately after birth. Pediatr Neurosurg 45:114–118. https://doi.org/10.1159/000209285. PMID: 19307745
Kumar R, Singhal N (2007) Outcome of meningomyelocele/lipomeningomyelocele in children of northern India. Pediatr Neurosurg 43(1):7–14. https://doi.org/10.1159/000097518. PMID: 17190981
McDowell MM, Lee PS, Foster KA et al (2018) The use of external ventricular drainage to reduce the frequency of wound complications in myelomeningocele closure. Pediatr Neurosurg 53(2):100–107. https://doi.org/10.1159/000485251. PMID: 29316543
Kshettry VR, Kelly ML, Rosenbaum BP, Seicean A, Hwang L, Weil RJ (2014) Myelomeningocele: Surgical trends and predictors of outcome in the United States, 1988–2010. J Neurosurg Pediatr 13(6):666–678. https://doi.org/10.3171/2014.3.PEDS13597. PMID: 24702620
Kobraei EM, Ricci JA, Vasconez HC, Rinker BD (2014) A comparison of techniques for myelomeningocele defect closure in the neonatal period. Childs Nerv Syst 30(9):1535–1541. https://doi.org/10.1007/s00381-014-2430-7. PMID: 24802545
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Srijan Singh, Sushant Mane, Suhani Jain and Aditi Bajaj. The first draft of the manuscript was written by Srijan Singh and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Disclosures
Nothing to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author's summary
What is known: Neural tube defects (NTDs) are one of the common birth defects and lead to disability. The incidence of neural tube defects (NTDs) (of which myelomeningocele is the most common) varies based on ethnic, geographic, and nutritional factors.
What is new: Meningomyelocele (MMC) is the most common NTD in Western India with the most common location being the lower back, and most frequently associated defect being hydrocephalus. COVID pandemic and lockdowns had reduced access to antenatal care, which is a major contributory factor to reduced rates of prenatal diagnosis. The overall mortality in our series was four (26.5%) secondary to meningitis and respiratory compromise, which is slightly higher than other studies due to the fact that this study was conducted during the COVID era with poor follow-up and compliance of patients. This study highlights the importance of routine pre-pregnancy folic acid supplementation, antenatal diagnosis, early surgery and proper follow-up for improving outcomes and reducing long-term impairments in children with NTDs.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Singh, S., Mane, S., Jain, S. et al. Clinical presentation and outcomes of neonates born with neural tube defects- an experience from a level III B NICU in Western India. Childs Nerv Syst 40, 163–170 (2024). https://doi.org/10.1007/s00381-023-06078-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-023-06078-w