Abstract
Purpose
To compare two populations of brachial plexus palsies, one neonatal (NBPP) and the other traumatic (NNBPP) who underwent different nerve transfers, using the plasticity grading scale (PGS) for detecting differences in brain plasticity between both groups.
Methods
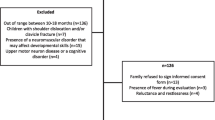
To be included, all patients had to have undergone a nerve transfer as the unique procedure to recover one lost function. The primary outcome was the PGS score. We also assessed patient compliance to rehabilitation using the rehabilitation quality scale (RQS). Statistical analysis of all variables was performed. A p ≤ 0.050 set as criterion for statistical significance.
Results
A total of 153 NNBPP patients and 35 NBPP babies (with 38 nerve transfers) met the inclusion criteria. The mean age at surgery of the NBPP group was 9 months (SD 5.42, range 4 to 23 months). The mean age of NNBPP patients was 22 years (SD 12 years, range 3 to 69). They were operated around sixth months after the trauma. All transfers performed in NBPP patients had a maximum PGS score of 4. This was not the case for the NNBPP population that reached a PGS score of 4 in approximately 20% of the cases. This difference was statistically significant (p < 0.001). The RQS was not significantly different between groups.
Conclusion
We found that babies with NBPP have a significantly greater capacity for plastic rewiring than adults with NNBPP. The brain in the very young patient can process the changes induced by the peripheral nerve transfer better than in adults.


Similar content being viewed by others
References
Malessy MJ, Pondaag W (2009) Obstetric brachial plexus injuries. Neurosurg Clin N Am 20(1):1–14. https://doi.org/10.1016/j.nec.2008.07.024
Socolovsky M, Martins RS, Di Masi G, Siqueira M (2012) Upper brachial plexus injuries: grafts vs ulnar fascicle transfer to restore biceps muscle function. Neurosurgery 71(2 Suppl Operative):ons 227–232. https://doi.org/10.1227/NEU.0b013e3182684b51
Socolovsky M, Barillaro K, Bonilla G, Di Masi G, Malessy M (2022) Nerve transfers for brachial plexus injuries: grading of volitional control. J Neurosurg 138(5):1419–1425. https://doi.org/10.3171/2022.7.JNS22887
Groen JL, Pondaag W, Malessy MJA (2023) Early grafting in severe adult traumatic brachial plexus injury. Neurosurg Focus Video 8(1):V13. https://doi.org/10.3171/2022.10.FOCVID2288
Khu KJ (2015) Neuroplasticity and brachial plexus injury. World Neurosurg 84(6):1509–1510. https://doi.org/10.1016/j.wneu.2015.06.065
Tuna Z, Oskay D, Algin O, Koçak OM (2020) Cortical motor areas show different reorganizational changes in adult patients with brachial plexus birth injury (BPBI). Int J Dev Neurosci 118:419–422. https://doi.org/10.1002/jdn.10037
de Sousa AC, Guedes-Corrêa JF (2016) Post-Oberlin procedure cortical neuroplasticity in traumatic injury of the upper brachial plexus. Radiol Bras 49(3):201–202. https://doi.org/10.1590/0100-3984.2015.0082
Bhat DI, Indira Devi B, Bharti K, Panda R (2017) Cortical plasticity after brachial plexus injury and repair: a resting-state functional MRI study. Neurosurg Focus 42(3):E14. https://doi.org/10.3171/2016.12.FOCUS16430
Socolovsky M, Malessy M, Lopez D, Guedes F, Flores L (2017) Current concepts in plasticity and nerve transfers: relationship between surgical techniques and outcomes. Neurosurg Focus 42(3):E13. https://doi.org/10.3171/2016.12.FOCUS16431
Chuieng-Yi Lu J, An-Jou Lin J, Lee CS, Nai-Jen Chang T, Chwei-Chin Chuang D (2022) Phrenic nerve as an alternative donor for nerve transfer to restore shoulder abduction in severe multiple root injuries of the adult brachial plexus. J Hand Surg Am 21:S0363–5023(22)00154. https://doi.org/10.1016/j.jhsa.2022.03.004
Socolovsky M, Malessy M, Bonilla G, Di Masi G, Conti ME, Lovaglio A (2018) Phrenic to musculocutaneous nerve transfer for traumatic brachial plexus injuries: analyzing respiratory effects on elbow flexion control. J Neurosurg 131(1):165–174. https://doi.org/10.3171/2018.4.JNS173248
Socolovsky M, Lovaglio A, Bonilla G, Di Masi G, Barillaro K, Malessy M (2023) Brain plasticity and age after restoration of elbow flexion with distal nerve transfers in neonatal brachial plexus palsy and traumatic brachial plexus injury using the plasticity grading scale. J Neurosurg In press
Socolovsky M, Di Masi G, Bonilla G, Lovaglio A, Krishnan KG (2021) Nerve graft length and recovery of elbow flexion muscle strength in patients with traumatic brachial plexus injuries: case series. Oper Neurosurg (Hagerstown) 20(6):521–528. https://doi.org/10.1093/ons/opab007
Flores LP, Socolovsky M (2016) Phrenic nerve transfer for reconstruction of elbow extension in severe brachial plexus injuries. J Reconstr Microsurg 32(7):546–550. https://doi.org/10.1055/s-0036-1583302
Socolovsky M, Di Masi G, Bonilla G, Domínguez Paez M, Robla J, Calvache Cabrera C (2015) The phrenic nerve as a donor for brachial plexus injuries: is it safe and effective? Case series and literature analysis. Acta Neurochir 157(6):1077–1086. https://doi.org/10.1007/s00701-015-2387-7
Solanki C, Socolovsky M, Devi BI, Bhat DI (2019) Nerve repair: bridging the gap from “limp” to “limb.” Neurol India 67(Supplement):S16–S19. https://doi.org/10.4103/0028-3886.250712
Kim D, Murovic J, Kline D (2004) Mechanisms of injury in operative brachial plexus lesions. Neurosurg Focus 16(5):E2-11
Estrella EP, Mina JE, Montales TD (2023) The outcome of single versus double nerve transfers in shoulder reconstruction of upper and extended upper-type brachial plexus injuries. J Hand Surg Glob Online 5(3):284–289. https://doi.org/10.1016/j.jhsg.2023.01.012
Javeed S, Greenberg JK, Zhang JK, Plog B, Dibble CF, Benedict B, Botterbush K, Khalifeh JM, Wen H, Chen Y, Park Y, Belzberg AJ, Tuffaha S, Burks SS, Levi AD, Zager EL, Faraji AH, Mahan MA, Midha R, Wilson TJ (2023) Association of upper-limb neurological recovery with functional outcomes in high cervical spinal cord injury. J Neurosurg Spine 1–8. https://doi.org/10.3171/2023.4.SPINE2382
Shin AY, Socolovsky M, Desai K, Fox M, Wang S, Spinner RJ (2022) Differences in management and treatment of traumatic adult pan brachial plexus injuries: a global perspective regarding continental variations. J Hand Surg Eur 47(1):40–51. https://doi.org/10.1177/17531934211039677
Socolovsky M, Costales JR, Paez MD, Nizzo G, Valbuena S, Varone E (2016) Obstetric brachial plexus palsy: reviewing the literature comparing the results of primary versus secondary surgery. Childs Nerv Syst 32(3):415–425. https://doi.org/10.1007/s00381-015-2971-4
Stroh AL, Grin K, Rösler F, Bottari D, Ossandón J, Rossion B, Röder B (2022) Developmental experiences alter the temporal processing characteristics of the visual cortex: evidence from deaf and hearing native signers. Eur J Neurosci 55(6):1629–1644. https://doi.org/10.1111/ejn.15629
Socolovsky M, Malessy M (2021) Brain changes after peripheral nerve repair: limitations of neuroplasticity. J Neurosurg Sci 65(4):421–430. https://doi.org/10.23736/S0390-5616.21.05298-X
Fraiman D, Miranda MF, Erthal F, Buur PF, Elschot M, Souza L, Rombouts SA, Schimmelpenninck CA, Norris DG, Malessy MJ, Galves A, Vargas CD (2016) Reduced functional connectivity within the primary motor cortex of patients with brachial plexus injury. Neuroimage Clin 12:277–284. https://doi.org/10.1016/j.nicl.2016.07.008
Eggers R, Tannemaat MR, De Winter F, Malessy MJ, Verhaagen J (2016) Clinical and neurobiological advances in promoting regeneration of the ventral root avulsion lesion. Eur J Neurosci 43(3):318–335. https://doi.org/10.1111/ejn.13089
Gawi EM (2011) The effects of age factor on learning English: a case study of learning English in Saudi schools, Saudi Arabia. Engl Lang Teach 5:127–139. https://doi.org/10.5539/elt.v5n1p127
Van der Looven (2021) Risk management, nerve regeneration and developing brain plasticity. Thesis submitted to fulfill the requirements for the degree of ‘doctor in medical sciences’ Ghent University, Belgium Juni
Auer T, Pinter S, Kovacs N, Kalmar Z, Nagy F, Horvath R, Koszo B, Kotek G, Perlaki G, Koves M, Kalman B, Komoly S, Schwarcz A, Woermann F (2009) Does obstetric brachial plexus injury influence speech dominance? Ann Neurol 65(1):57–66. https://doi.org/10.1002/ana.21538
Kolb B, Harker A, Gibb R (2017) Principles of plasticity in the developing brain. Dev Med Child Neurol 59(12):1218–1223. https://doi.org/10.1111/dmcn.13546
Siero JCW, Hermes D, Hoogduin H, Luijten PR, Ramsey NF, Petridou N (2014) BOLD matches neuronal activity at the mm scale: a combined 7 T fMRI and ECoG study in human sensorimotor cortex. Neuroimage 101:177–184. https://doi.org/10.1016/j.neuroimage.2014.07.002
Siebner HR, Rothwell J (2003) Transcranial magnetic stimulation: new insights into representational cortical plasticity. Exp Brain res 148(1):1–16. https://doi.org/10.1007/s00221-002-1234-2
Li S, HanY WD, Yang H, Fan Y, Lv Y, Tang H, Gong Q, Zang Y, He Y (2010) Mapping surface variability of the central sulcus in musicians. Cereb cortex 20(1):25–33. https://doi.org/10.1093/cercor/bhp074
Socolovsky M, Di Masi G, Battaglia D (2011) Use of long autologous nerve grafts in brachial plexus reconstruction: factors that affect the outcome. Acta Neurochir (Wien) 153(11):2231–2240. https://doi.org/10.1007/s00701-011-1131-1
Estrada RG, Bacca J, Socolovsky M (2021) A novel dual nerve transfer for restoration of shoulder function and sensory recovery of the hand, in patients with C567 traumatic root avulsion of the brachial plexus. Clin Neurol Neurosurg 210:107005. https://doi.org/10.1016/j.clineuro.2021.107005
Faglioni W Jr, Siqueira MG, Martins RS, Heise CO, Foroni L (2014) The epidemiology of adult traumatic brachial plexus lesions in a large metropolis. Acta Neurochir (Wien) 156(5):1025–1028. https://doi.org/10.1007/s00701-013-1948-x
Fu SY, Gordon T (1995) Contributing factors to poor functional recovery after delayed nerve repair: prolonged axotomy. J Neurosci 15(5 Pt 2):3876–3885. https://doi.org/10.1523/JNEUROSCI.15-05-03876.1995
Pondaag W, Malessy MJ (2014) The evidence for nerve repair in obstetric brachial plexus palsy revisited. Biomed Res Int 2014:434619. https://doi.org/10.1155/2014/434619
Author information
Authors and Affiliations
Contributions
Conception and design: MS, GdM, and MM. Acquisition of data: DB, MS, AL, GdM, and GB. Analysis and interpretation of data: all authors. Drafting the article: MS, MM, and RR. Critically revising the article: MM and MS.
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflicts of interest concerning the materials or methods used in this study or the findings reported in this paper. No funding, grants, and financial or non-financial interests were involved directly or indirectly related to the work submitted for publication. All ethical standards than could be related during design, data collection, statistical analysis, writing, and editing this paper were accomplished, as well as any treatment of personal data from the patients involved.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Socolovsky, M., di Masi, G., Bonilla, G. et al. Brain plasticity in neonatal brachial plexus palsies: quantification and comparison with adults’ brachial plexus injuries. Childs Nerv Syst 40, 479–486 (2024). https://doi.org/10.1007/s00381-023-06072-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-023-06072-2