Abstract
Purpose
The most important complication of paravertebral tumors is cord compression (CC), which is an oncologic emergency. Early and appropriate intervention is important in terms of reducing morbidity and mortality. Here, we report our clinical experience with paravertebral tumors.
Methods
The files of patients who were followed up for benign/malignant paravertebral tumors between 1988 and 2022 were evaluated retrospectively.
Results
There were 96 patients with paravertebral tumors. The median age at diagnosis was 5 years (1 month–17 years). The male/female ratio was 1.13. The median time to diagnosis was 4 weeks (0–28 weeks). The most common presenting complaint was pain (62.5%). The diagnosis distribution was as follows: sympathetic nervous system (SNS) tumors (n: 38), soft tissue sarcomas (STS) (n: 23), Langerhans cell histiocytosis (LCH) (n: 12), central nervous system (CNS) tumors (n: 9), germ cell tumor (n: 6), lymphomas (n: 4), and benign tumors (n: 4). Sixty-five patients (67.7%) had CC, 40% of whom received chemotherapy as first-line treatment. Decompression surgery was performed in 58.5% of the patients. For patients with CC, 26 patients had advanced disease at admission. Serious neurologic sequelae were observed in seventeen (17.7%) patients.
Conclusion
Pain and neurological findings in childhood are warning signs for paravertebral tumors and CC. A detailed neurologic examination and radiodiagnostic imaging should be performed, and a definitive diagnosis should be made quickly. Anticancer treatment should be planned multidisciplinary. Decompression surgery should be discussed for patients with severe neurological deficits. Childhood cancers are chemosensitive; if possible, treatment should be initiated with chemotherapy to avoid neurological sequelae.





Similar content being viewed by others
Data availability
Data can be available from corresponding author.
Abbreviations
- CC:
-
Cord compression
- SNS:
-
Sympathetic nervous system
- STS:
-
Soft tissue sarcomas
- LCH:
-
Langerhans cell histiocytosis
- CNS:
-
Central nervous system
- CT:
-
Computerized tomography
- MRI:
-
Magnetic resonance imaging
- CR:
-
Complete remission
- NHL:
-
Non-Hodgkin lymphoma
- HL:
-
Hodgkin lymphoma
- RT:
-
Radiotherapy
References
Gunes D, Uysal KM, Cetinkaya H, Tekin HG, Yuceer N, Sarialioglu F, Olgun N (2009) Paravertebral malignant tumors of childhood: analysis of 28 pediatric patients. Childs Nerv Syst 25:63–69
Sorrentino S, Ash S, Haupt R, Plantaz D, Schiff I, Hero B, Simon T, Kachanov D, Shamanskaya T, Kraal K, Littooij A, Wieczoreck A, Balwierz W, Laureys G, Trager C, Sertorio F, Erminio G, Fragola M, Beck Popovic M, De Bernardi B, Trahair T (2022) Presenting features of neuroblastoma with spinal canal invasion. A prospective study of the International Society of Pediatric Oncology Europe - Neuroblastoma (SIOPEN). Front Pediatr 10:1023498
Sun H, Nemecek AN (2010) Optimal management of malignant epidural spinal cord compression. Hematol Oncol Clin North Am 24:537–551
Pizzo PA PD (2021) Oncologic emergencies, Philadelphia
Raffel C, Neave VC, Lavine S, McComb JG (1991) Treatment of spinal cord compression by epidural malignancy in childhood. Neurosurg 28:349–352
De Martino L, Spennato P, Vetrella S, Capasso M, Porfito C, Ruotolo S, Abate ME, Cinalli G, Quaglietta L (2019) Symptomatic malignant spinal cord compression in children: a single-center experience. Ital J Pediatr 45:80
Pollono D, Tomarchia S, Drut R, Ibanez O, Ferreyra M, Cedola J (2003) Spinal cord compression: a review of 70 pediatric patients. Pediatr Hematol Oncol 20:457–466
Tantawy AA, Ebeid FS, Mahmoud MA, Shepl OE (2013) Spinal cord compression in childhood pediatric malignancies: multicenter Egyptian study. J Pediatr Hematol Oncol 35:232–236
Angelini P, Plantaz D, De Bernardi B, Passagia JG, Rubie H, Pastore G (2011) Late sequelae of symptomatic epidural compression in children with localized neuroblastoma. Pediatr Blood Cancer 57:473–480
Plantaz D, Rubie H, Michon J, Mechinaud F, Coze C, Chastagner P, Frappaz D, Gigaud M, Passagia JG, Hartmann O (1996) The treatment of neuroblastoma with intraspinal extension with chemotherapy followed by surgical removal of residual disease. A prospective study of 42 patients–results of the NBL 90 Study of the French Society of Pediatric Oncology. Cancer 78:311–319
Katzenstein HM, Kent PM, London WB, Cohn SL (2001) Treatment and outcome of 83 children with intraspinal neuroblastoma: the Pediatric Oncology Group experience. J Clin Oncol 19:1047–1055
Simon T, Niemann CA, Hero B, Henze G, Suttorp M, Schilling FH, Berthold F (2012) Short- and long-term outcome of patients with symptoms of spinal cord compression by neuroblastoma. Dev Med Child Neurol 54:347–352
Punt J, Pritchard J, Pincott JR, Till K (1980) Neuroblastoma: a review of 21 cases presenting with spinal cord compression. Cancer 45:3095–3101
Holgersen LO, Santulli TV, Schullinger JN, Berdon WE (1983) Neuroblastoma with intraspinal (dumbbell) extension. J Pediatr Surg 18:406–411
Kraal K, Blom T, Tytgat L, van Santen H, van Noesel M, Smets A, Bramer J, Caron H, Kremer L, van der Pal H (2016) Neuroblastoma with intraspinal extension: health problems in long-term survivors. Pediatr Blood Cancer 63:990–996
De Bernardi B, Pianca C, Pistamiglio P, Veneselli E, Viscardi E, Pession A, Alvisi P, Carli M, Donfrancesco A, Casale F, Giuliano MG, di Montezemolo LC, Di Cataldo A, Lo Curto M, Bagnulo S, Schumacher RF, Tamburini A, Garaventa A, Clemente L, Bruzzi P (2001) Neuroblastoma with symptomatic spinal cord compression at diagnosis: treatment and results with 76 cases. J Clin Oncol 19:183–190
Aydin GB, Kutluk MT, Buyukpamukcu M, Akyuz C, Yalcin B, Varan A (2010) Neurological complications of neuroblastic tumors: experience of a single center. Childs Nerv Syst 26:359–365
Pio L, Blanc T, de Saint DT, Irtan S, Valteau-Couanet D, Michon J, Brisse H, Galmiche-Rolland L, Joyeux L, Odent T, Harte C, Glorion C, Zerah M, Sarnacki S (2019) Multidisciplinary surgical strategy for dumbbell neuroblastoma: a single-center experience of 32 cases. Pediatr Blood Cancer 66(Suppl 3):e27670
De Bernardi B, Balwierz W, Bejent J, Cohn SL, Garre ML, Iehara T, Plantaz D, Simon T, Angelini P, Cama A, London WB, Kramer K, Katzenstein HM, Tortori-Donati P, Rossi A, D’Angio GJ, Evans AE (2005) Epidural compression in neuroblastoma: diagnostic and therapeutic aspects. Cancer Lett 228:283–299
Hayes FA, Thompson EI, Hvizdala E, O’Connor D, Green AA (1984) Chemotherapy as an alternative to laminectomy and radiation in the management of epidural tumor. J Pediatr 104:221–224
Sanderson IR, Pritchard J, Marsh HT (1989) Chemotherapy as the initial treatment of spinal cord compression due to disseminated neuroblastoma. J Neurosurg 70:688–690
Hoover M, Bowman LC, Crawford SE, Stack C, Donaldson JS, Grayhack JJ, Tomita T, Cohn SL (1999) Long-term outcome of patients with intraspinal neuroblastoma. Med Pediatr Oncol 32:353–359
Fawzy M, El-Beltagy M, Shafei ME, Zaghloul MS, Kinaai NA, Refaat A, Azmy S (2015) Intraspinal neuroblastoma: treatment options and neurological outcome of spinal cord compression. Oncol Lett 9:907–911
Mirzaei L, Kaal SE, Schreuder HW, Bartels RH (2015) The neurological compromised spine due to Ewing sarcoma. What first: surgery or chemotherapy? Therapy, survival, and neurological outcome of 15 cases with primary Ewing sarcoma of the vertebral column. Neurosurg 77:718–724; discussion 724–715
Xu X, Han S, Jiang L, Yang S, Liu X, Yuan H, Wei F, Wu F, Dang L, Zhou H, Zhang H, Liu Z (2018) Clinical features and treatment outcomes of Langerhans cell histiocytosis of the spine. Spine J 18:1755–1762
Ince D, Demirag B, Ozek G, Erbay A, Ortac R, Oymak Y, Kamer S, Yaman Y, Kundak S, Vergin C (2016) Pediatric Langerhans cell histiocytosis: single center experience over a 17-year period. Turk J Pediatr 58:349–355
Mora J, Wollner N (1999) Primary epidural non-Hodgkin lymphoma: spinal cord compression syndrome as the initial form of presentation in childhood non-Hodgkin lymphoma. Med Pediatr Oncol 32:102–105
Kurucu N, Akyuz C, Varan A, Akcoren Z, Aydin B, Yalcin B, Kutluk T (2021) Primary paraspinal and spinal epidural non-Hodgkin lymphoma in childhood. J Pediatr Hematol Oncol 43:e395–e400
Seilern Und Aspang J, Burnand KM, Ong H, Cross K, Thompson D, Giuliani S (2020) Sacrococcygeal teratoma with intraspinal extension: a case series and review of literature. J Pediatr Surg 55:2022–2025
Author information
Authors and Affiliations
Contributions
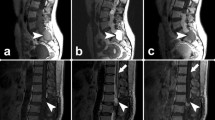
Deniz Kizmazoglu, Dilek Ince, and Nur Olgun wrote the main manuscript. Emre Cecen and Ceren Kizmazoglu discussed the literature. Handan Guleryuz prepared the figures. Erdener Ozer prepared the data about pathology. Ayse Demiral prepared the data for radiotheraphy. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kizmazoglu, D., Ince, D., Cecen, E. et al. Pediatric paravertebral tumors: analysis of 96 patients. Childs Nerv Syst 40, 123–133 (2024). https://doi.org/10.1007/s00381-023-06064-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-023-06064-2