Abstract
Purpose
Cerebrospinal fluid (CSF) shunt failures in children are devastating. The primary aims of this study are to, firstly, review our institutional series of ventriculoperitoneal shunt (VPS) insertions and identify factors associated with shunt failure.
Methods
This is a single-institution, retrospective study conducted over a 12-year period. All patients under 18 years old with VPS inserted were included. Variables of interest such as patient characteristics, hydrocephalus aetiology, shunt implant details, and outcomes were subjected to statistical analyses.
Results
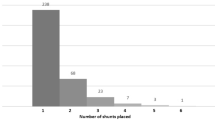
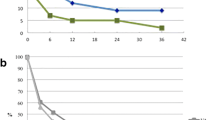
A total of 214 VPS patients were selected for this study. The mean age at VPS insertion was 6 months with a mean follow-up duration of 44 months. The most common type of hydrocephalus was obstructive (n = 142, 66.4%), and the most frequent aetiology was tumour-related (n = 66, 30.8%). The 30-day shunt failure rate was 9.3%: 9 infections (4.2%), 7 occlusions (3.3%), and 4 others (1.9%). After multivariable analysis, only recent central nervous system (CNS) infection prior to VPS insertion remained significant (OR 15.4 (1.3–175), p = 0.028).
Conclusion
This is the first, large-scale local study focused on the shunt failure in Singaporean children. Significant findings in our study demonstrate that recently treated CNS infection is a factor associated with 30-day shunt failure while the values of CSF constituents were not contributory.


Similar content being viewed by others
Availability of data and materials
All data generated or analysed during this study are included in this published article and supplementary material.
References
Isaacs AM, Riva-Cambrin J, Yavin D, Hockley A, Pringsheim TM, Jette N, Lethebe BC, Lowerison M, Dronyk J, Hamilton MG (2018) Age-specific global epidemiology of hydrocephalus: systematic review, metanalysis and global birth surveillance. PLoS ONE 13:e0204926
Lee RP, Ajmera S, Thomas F, Dave P, Lillard JC, Wallace D, Broussard A, Motiwala M, Norrdahl SP, Venable GT, Khan NR, Harrell C, Jones TL, Vaughn BN, Gooldy T, Hersh DS, Klimo P (2020) Shunt failure-the first 30 days. Neurosurgery 87:123–129
Venable GT, Rossi NB, Morgan Jones G, Khan NR, Smalley ZS, Roberts ML, Klimo P Jr (2016) The preventable shunt revision rate: a potential quality metric for pediatric shunt surgery. J Neurosurg Pediatr 18:7–15
Lee L, Low S, Low D, Ng LP, Nolan C, Seow WT (2016) Late pediatric ventriculoperitoneal shunt failures: a Singapore tertiary institution’s experience. Neurosurg Focus 41:E7
Lam SK, Srinivasan VM, Luerssen TG, Pan IW (2014) Cerebrospinal fluid shunt placement in the pediatric population: a model of hospitalization cost. Neurosurg Focus 37:E5
Simon TD, Riva-Cambrin J, Srivastava R, Bratton SL, Dean JM, Kestle JR, Hydrocephalus Clinical Research N (2008) Hospital care for children with hydrocephalus in the United States: utilization, charges, comorbidities, and deaths. J Neurosurg Pediatr 1:131–137
Chotai S, Guidry BS, Chan EW, Sborov KD, Gannon S, Shannon C, Bonfield CM, Wellons JC, Naftel RP (2017) Unplanned readmission within 90 days after pediatric neurosurgery. J Neurosurg Pediatr 20:542–548
Kaestner S, Sani R, Graf K, Uhl E, Godau J, Deinsberger W (2021) CSF shunt valve occlusion-does CSF protein and cell count matter? Acta Neurochir (Wien) 163:1991–1996
Cheatle JT, Bowder AN, Tefft JL, Agrawal SK, Hellbusch LC (2015) Effect of protein concentration on the flow of cerebrospinal fluid through shunt tubing. Neurosurgery 77:972–978
Brydon HL, Hayward R, Harkness W, Bayston R (1995) Physical properties of cerebrospinal fluid of relevance to shunt function. 2: The effect of protein upon CSF surface tension and contact angle. Br J Neurosurg 9:645–651
Brydon HL, Hayward R, Harkness W, Bayston R (1995) Physical properties of cerebrospinal fluid of relevance to shunt function. 1: The effect of protein upon CSF viscosity. Br J Neurosurg 9:639–644
Riva-Cambrin J, Kestle JR, Holubkov R, Butler J, Kulkarni AV, Drake J, Whitehead WE, Wellons JC, 3rd, Shannon CN, Tamber MS, Limbrick DD, Jr., Rozzelle C, Browd SR, Simon TD, Hydrocephalus Clinical Research N (2016) Risk factors for shunt malfunction in pediatric hydrocephalus: a multicenter prospective cohort study. J Neurosurg Pediatr 17:382–390
Hanak BW, Bonow RH, Harris CA, Browd SR (2017) Cerebrospinal fluid shunting complications in children. Pediatr Neurosurg 52:381–400
Hasanain AA, Abdullah A, Alsawy MFM, Soliman MAR, Ghaleb AA, Elwy R, Ezzat AAM, Al Menabbawy A, Marei AA, Abd El Razik B, El Hamaky MI, Schroeder HWS, Fleck S, El Damaty A, Marx S, Nowak S, Baldauf J, Zohdi A, El Refaee EA (2019) Incidence of and causes for ventriculoperitoneal shunt failure in children younger than 2 years: a systematic review. J Neurol Surg A Cent Eur Neurosurg 80:26–33
Kestle JR, Riva-Cambrin J, Wellons JC, 3rd, Kulkarni AV, Whitehead WE, Walker ML, Oakes WJ, Drake JM, Luerssen TG, Simon TD, Holubkov R, Hydrocephalus Clinical Research N (2011) A standardized protocol to reduce cerebrospinal fluid shunt infection: the Hydrocephalus Clinical Research Network Quality Improvement Initiative. J Neurosurg Pediatr 8:22–29
Morota N (2017) Complex hydrocephalus: management by “Smart Shunt.” In: Ammar A (ed) Hydrocephalus: what do we know? And what do we still not know? Springer International Publishing, Cham, pp 259–280
Zuccaro G, Ramos JG (2011) Multiloculated hydrocephalus. Childs Nerv Syst 27:1609–1619
Akbari SH, Holekamp TF, Murphy TM, Mercer D, Leonard JR, Smyth MD, Park TS, Limbrick DD Jr (2015) Surgical management of complex multiloculated hydrocephalus in infants and children. Childs Nerv Syst 31:243–249
Sciubba DM, Stuart RM, McGirt MJ, Woodworth GF, Samdani A, Carson B, Jallo GI (2005) Effect of antibiotic-impregnated shunt catheters in decreasing the incidence of shunt infection in the treatment of hydrocephalus. J Neurosurg 103:131–136
Eymann R, Steudel WI, Kiefer M (2009) Infection rate with application of an antibiotic-impregnated catheter for shunt implantation in children - a retrospective analysis. Klin Padiatr 221:69–73
Pattavilakom A, Xenos C, Bradfield O, Danks RA (2007) Reduction in shunt infection using antibiotic impregnated CSF shunt catheters: an Australian prospective study. J Clin Neurosci 14:526–531
Mortazavi MM, Adeeb N, Griessenauer CJ, Sheikh H, Shahidi S, Tubbs RI, Tubbs RS (2014) The ventricular system of the brain: a comprehensive review of its history, anatomy, histology, embryology, and surgical considerations. Childs Nerv Syst 30:19–35
Evans WA Jr (1942) An encephalographic ratio for estimating ventricular enlargement and cerebral atrophy. Arch Neurol Psychiatry 47:931–937
Harris CA, McAllister JP II (2011) Does drainage hole size influence adhesion on ventricular catheters? Childs Nerv Syst 27:1221–1232
Harris CA, Resau JH, Hudson EA, West RA, Moon C, Black AD, McAllister JP II (2011) Effects of surface wettability, flow, and protein concentration on macrophage and astrocyte adhesion in an in vitro model of central nervous system catheter obstruction. J Biomed Mater Res A 97:433–440
Al-Tamimi YZ, Sinha P, Chumas PD, Crimmins D, Drake J, Kestle J, British Pediatric Neurosurgery Group Audit C, Hayward R, Solanki GA, Thomson S, Thorne J (2014) Ventriculoperitoneal shunt 30-day failure rate: a retrospective international cohort study. Neurosurgery 74:29–34
Berry JG, Hall MA, Sharma V, Goumnerova L, Slonim AD, Shah SS (2008) A multi-institutional, 5-year analysis of initial and multiple ventricular shunt revisions in children. Neurosurgery 62: 445–453; discussion 453–444
Kestle J, Drake J, Milner R, Sainte-Rose C, Cinalli G, Boop F, Piatt J, Haines S, Schiff S, Cochrane D, Steinbok P, MacNeil N (2000) Long-term follow-up data from the Shunt Design Trial. Pediatr Neurosurg 33:230–236
Anderson IA, Saukila LF, Robins JMW, Akhunbay-Fudge CY, Goodden JR, Tyagi AK, Phillips N, Chumas PD (2018) Factors associated with 30-day ventriculoperitoneal shunt failure in pediatric and adult patients. J Neurosurg 130:145–153
Paudel P, Bista P, Pahari DP, Sharma GR (2020) Ventriculoperitoneal shunt complication in pediatric hydrocephalus: risk factor analysis from a single institution in Nepal. Asian J Neurosurg 15:83–87
Piatt JH Jr (2014) Thirty-day outcomes of cerebrospinal fluid shunt surgery: data from the National Surgical Quality Improvement Program-Pediatrics. J Neurosurg Pediatr 14:179–183
Tuli S, O'Hayon B, Drake J, Clarke M, Kestle J (1999) Change in ventricular size and effect of ventricular catheter placement in pediatric patients with shunted hydrocephalus. Neurosurgery 45: 1329–1333; discussion 1333–1325
Pillai SV (2021) Techniques and Nuances in Ventriculoperitoneal Shunt Surgery. Neurol India 69:S471–S475
Kraemer MR, Sandoval-Garcia C, Bragg T, Iskandar BJ (2017) Shunt-dependent hydrocephalus: management style among members of the American Society of Pediatric Neurosurgeons. J Neurosurg Pediatr 20:216–224
Yoon YK, Kim J, Moon C, Lee MS, Hur J, Lee H, Kim SW (2019) Antimicrobial susceptibility of microorganisms isolated from patients with intraabdominal infection in Korea: a multicenter study. J Korean Med Sci 34:e309
Skar GL, Synhorst D, Beaver M, Snowden JN (2019) CSF inflammatory markers differ in gram-positive versus gram-negative shunt infections. J Neuroinflammation 16:7
Kamat AS, Gretschel A, Vlok AJ, Solomons R (2018) CSF protein concentration associated with ventriculoperitoneal shunt obstruction in tuberculous meningitis. Int J Tuberc Lung Dis 22:788–792
Notarianni C, Vannemreddy P, Caldito G, Bollam P, Wylen E, Willis B, Nanda A (2009) Congenital hydrocephalus and ventriculoperitoneal shunts: influence of etiology and programmable shunts on revisions. J Neurosurg Pediatr 4:547–552
Yakut N, Soysal A, Kadayifci EK, Dalgic N, Ciftdogan DY, Karaaslan A, Cagan E, Celikboya E, Kanik A, Dagcinar A, Yilmaz A, Ozer F, Camlar M, Turel O, Bakir M (2016) Persistant high cerebrospinal fluid protein may be a risk factor for ventriculoperitoneal shunt reinfection in children. Open Forum Infectious Diseases 3
Pezzotta S, Locatelli D, Bonfanti N, Sfogliarini R, Bruschi L, Rondini G (1987) Shunt in high-risk newborns. Childs Nerv Syst 3:114–116
Laviv Y, Kasper BS, Kasper EM (2018) Vascular hyperpermeability as a hallmark of phacomatoses: is the etiology angiogenesis comparable with mechanisms seen in inflammatory pathways? Part I: historical observations and clinical perspectives on the etiology of increased CSF protein levels, CSF clotting, and communicating hydrocephalus: a comprehensive review. Neurosurg Rev 41:957–968
Fulkerson DH, Vachhrajani S, Bohnstedt BN, Patel NB, Patel AJ, Fox BD, Jea A, Boaz JC (2011) Analysis of the risk of shunt failure or infection related to cerebrospinal fluid cell count, protein level, and glucose levels in low-birth-weight premature infants with posthemorrhagic hydrocephalus. J Neurosurg Pediatr 7:147–151
Rammos S, Klopfenstein J, Augspurger L, Wang H, Wagenbach A, Poston J, Lanzino G (2008) Conversion of external ventricular drains to ventriculoperitoneal shunts after aneurysmal subarachnoid hemorrhage: effects of site and protein/red blood cell counts on shunt infection and malfunction. J Neurosurg 109:1001–1004
Jernigan SC, Berry JG, Graham DA, Goumnerova L (2014) The comparative effectiveness of ventricular shunt placement versus endoscopic third ventriculostomy for initial treatment of hydrocephalus in infants. J Neurosurg Pediatr 13:295–300
Rahman MM, Khan SIMKN, Khan RA, Islam R, Sarker MH (2021) Endoscopic third ventriculostomy in children: problems and surgical outcome: analysis of 34 cases. Chin Neurosurg J 7:3
Kulkarni AV, Drake JM, Mallucci CL, Sgouros S, Roth J, Constantini S (2009) Endoscopic third ventriculostomy in the treatment of childhood hydrocephalus. J Pediatr 155:254-259.e251
Javeed F, Mohan A, Wara UU, Rehman L, Khan M (2023) Ventriculoperitoneal shunt surgery for hydrocephalus: one of the common neurosurgical procedures and its related problems. Cureus 15:e35002
Abstracts from Hydrocephalus 2022: the Fourteenth Meeting of the Hydrocephalus Society (2023) Fluids Barriers CNS 19(Suppl 1):104
Hayhurst C, Beems T, Jenkinson MD, Byrne P, Clark S, Kandasamy J, Goodden J, Nandoe Tewarie RD, Mallucci CL (2010) Effect of electromagnetic-navigated shunt placement on failure rates: a prospective multicenter study. J Neurosurg 113:1273–1278
Author information
Authors and Affiliations
Contributions
All authors have read and approved the manuscript. Conceptualization: Jia Xu Lim, Sharon YY Low. Data curation: Lee Ping Ng, Hui Ping Han, Yi Wen Foo. Formal analysis: Yiong Huak Chan, Jia Xu Lim. Investigation: Yiong Huak Chan, Jia Xu Lim. Methodology: Jia Xu Lim, Sharon YY Low. Project administration: Sharon YY Low. Resources: David CY Low, Wan Tew Seow, Sharon YY Low. Validation: Yiong Huak Chan, Jia Xu Lim, Sharon YY Low. Writing—original draft: Jia Xu Lim. Writing—review and editing: Sharon YY Low.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study is approved by the hospital ethics review board (Reference: Singhealth CIRB 2020/2416). The consent to publish is included as part of the written, informed consent form in this study.
Consent for publication
Participants and/or their legal guardians signed a written consent for this study. The consent to publish has been included as part of the study.
Conflict of interests
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
381_2023_6007_MOESM1_ESM.docx
Supplementary file1 Supplementary Table 1: Adjusted CSF results for shunt occlusion and infection at timepoints of interest. (DOCX 16 KB)
381_2023_6007_MOESM2_ESM.docx
Supplementary file2 Supplementary Table 2: Summary of subgroup of patients with shunt infections. (Of note, ‘proximal infections’ are defined as infections of the ventricular catheter and/or shunt valve, while ‘distal infections’ are defined as infections of the peritoneal catheter). (DOCX 17 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lim, J.X., Han, H.P., Foo, Y.W. et al. Paediatric ventriculoperitoneal shunt failures: 12-year experience from a Singapore children’s hospital. Childs Nerv Syst 39, 3445–3455 (2023). https://doi.org/10.1007/s00381-023-06007-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-023-06007-x