Abstract
Purpose
To evaluate clinical and imaging characteristics of pediatric brain aneurysms.
Materials and Methods
A retrospective review of 1458 MR angiograms of pediatric patients (≤18 years old) obtained between 2006 and 2021 was performed. A non-infundibular arterial luminal outpouching larger than 1mm in size was identified as an “Intracranial aneurysm.” Patient demographics, clinical presentations, and predisposing risk factors, including family history and underlying medical conditions, were reviewed. MRA images were analyzed for aneurysm location, number, maximum diameter, and interval changes on follow-up.
Results
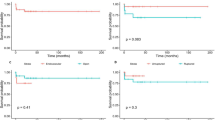
Forty-nine (3.3%) patients (30 females, 19 males) with 64 intracranial aneurysms were identified with an average age of 13.71 ± 3.67 years. Eleven (22.4%) patients had multiple aneurysms. An underlying systemic illness was observed in 81.6% (40/49) cases, with sickle cell disease as the most frequent (25/49, 51%) diagnosis. A first-degree family history of intracranial aneurysms was recognized in 36/1458 (2.5%) patients. However, no intracranial aneurysm was found in this group. While 02/49 (4%) patients presented with acute SAH, headache was the most common (16/49, 32.7%) symptom at presentation in unruptured cases. The majority (47/64, 73.4%) of the aneurysms were located in the anterior circulation, with the ICA ophthalmic segment being most frequently (24/47, 51%) involved. Most (54/64, 84.4%) aneurysms were smaller than 4mm in size at the time of diagnosis. At least one follow-up MRA was obtained in 72.3% (34/47) of the unruptured aneurysms cohort. There was no change in the aneurysm size and morphology in 31/34 (91.2 %) patients over an average imaging follow-up of 39.6 months. Three (6%) patients demonstrated an interval increase in the aneurysm size. SAH patients (n=2) and two unruptured aneurysm patients with an interval increase in size were successfully treated with endovascular techniques.
Conclusion
Female predominance with a higher frequency of small and unruptured intracranial aneurysms was recognized in our cohort. A higher incidence of an underlying systemic illness, especially sickle cell disease, was also noted. Most intracranial aneurysms in children appear to remain stable. However, there seems to be the risk of an aneurysm size increase which warrants regular clinical and imaging follow-up.


Similar content being viewed by others
Data availability
The data that support the findings of this study are available on request from the corresponding author, [SKL]. The data are not publicly available due to their containing information that could compromise the privacy of research participants.
References
Agid R, Jonas Kimchi T, Lee SK, Ter Brugge KG (2007) Diagnostic characteristics and management of intracranial aneurysms in children. Neuroimaging Clin N Am 17(2):153–163. https://doi.org/10.1016/j.nic.2007.02.001
Vaid VK, Kumar R, Kalra SK, Mahapatra AK, Jain VK (2008) Pediatric intracranial aneurysms: an institutional experience. Pediatr Neurosurg 44(4):296–301. https://doi.org/10.1159/000131678
Deora H, Rao KVLN, Somanna S, Srinivas D, Shukla DP, Bhat DI (2017) Surgically Managed Pediatric Intracranial Aneurysms: How Different Are They from Adult Intracranial Aneurysms? Pediatr Neurosurg 52(5):313–317. https://doi.org/10.1159/000477815
Mehrotra A, Nair AP, Das KK, Srivastava A, Sahu RN, Kumar R (2012) Clinical and radiological profiles and outcomes in pediatric patients with intracranial aneurysms. J Neurosurg Pediatr 10(4):340–346. https://doi.org/10.3171/2012.7.PEDS11455
Xu R, Xie ME, Yang W et al (2021) Epidemiology and outcomes of pediatric intracranial aneurysms: comparison with an adult population in a 30-year, prospective database [published online ahead of print, 2021 Sep 10]. J Neurosurg Pediatr 1–10. https://doi.org/10.3171/2021.6.PEDS21268
Hetts SW, Narvid J, Sanai N et al (2009) Intracranial aneurysms in childhood: 27-year single-institution experience. AJNR Am J Neuroradiol 30(7):1315–1324. https://doi.org/10.3174/ajnr.A1587
Bisson DA, Dirks P, Amirabadi A et al (2019) Unruptured intracranial aneurysms in children: 18 years' experience in a tertiary care pediatric institution. J Neurosurg Pediatr 24(2):184–189. Published 2019 May 24. https://doi.org/10.3171/2019.4.PEDS18703
Vasan R, Patel J, Sweeney JM et al (2013) Pediatric intracranial aneurysms: current national trends in patient management and treatment. Childs Nerv Syst 29(3):451–456. https://doi.org/10.1007/s00381-012-1945-z
Nabavizadeh SA, Vossough A, Ichord RN et al (2016) Intracranial aneurysms in sickle cell anemia: clinical and imaging findings. J Neurointerv Surg 8(4):434–440. https://doi.org/10.1136/neurintsurg-2014-011572
Saini S, Speller-Brown B, Wyse E et al (2015) Unruptured intracranial aneurysms in children with sickle cell disease: analysis of 18 aneurysms in 5 patients. Neurosurgery 76(5):531–539. https://doi.org/10.1227/NEU.0000000000000670
Preul MC, Cendes F, Just N, Mohr G (1998) Intracranial aneurysms and sickle cell anemia: multiplicity and propensity for the vertebrobasilar territory. Neurosurgery 42(5):971–978. https://doi.org/10.1097/00006123-199805000-00007
Garg K, Singh PK, Sharma BS et al (2014) Pediatric intracranial aneurysms–our experience and review of literature. Childs Nerv Syst 30(5):873–883. https://doi.org/10.1007/s00381-013-2336-9
Feng X, Ji W, Qian Z, Liu P, Kang H, Wen X et al (2017) Bifurcation location is significantly associated with rupture of small intracranial aneurysms (<5 mm). World Neurosurg 98:538–45. https://doi.org/10.1016/j.wneu.2016.11.055
Hassan T, Timofeev EV, Saito T, Shimizu H, Ezura M, Matsumoto Y et al (2005) A proposed parent vessel geometry-based categorization of saccular intracranial aneurysms: computational flow dynamics analysis of the risk factors for lesion rupture. J Neurosurg 103:662–80. https://doi.org/10.3171/jns.2005.103.4.0662
Liu Q, Jiang P, Jiang Y et al (2019) Bifurcation Configuration Is an Independent Risk Factor for Aneurysm Rupture Irrespective of Location. Front Neurol. 10:844. Published 2019 Aug 6. https://doi.org/10.3389/fneur.2019.00844
Huguenard AL, Gupta VP, Braverman AC, Dacey RG (2021) Genetic and heritable considerations in patients or families with both intracranial and extracranial aneurysms. J Neurosurg 134(6):1999–2006. Published 2021 Jan 1. https://doi.org/10.3171/2020.8.JNS203234
Brown RD Jr, Huston J, Hornung R et al (2008) Screening for brain aneurysm in the Familial Intracranial Aneurysm study: frequency and predictors of lesion detection. J Neurosurg 108(6):1132–1138. https://doi.org/10.3171/JNS/2008/108/6/1132
Crawley F, Clifton A, Brown MM (1999) Should we screen for familial intracranial aneurysm? Stroke 30(2):312–316. https://doi.org/10.1161/01.str.30.2.312
Asaithambi G, Adil MM, Shah KM, Jordan LC, Qureshi AI (2014) Patterns of treatment and associated short-term outcomes of unruptured intracranial aneurysms in children. Childs Nerv Syst 30(10):1697–1700. https://doi.org/10.1007/s00381-014-2423-6
Author information
Authors and Affiliations
Contributions
Conception of the work: SKL and DK; Data Collection: DK, RZ, SB, AT, and RH; Data analysis and interpretation: SKL, DK, RZ, and SB; Drafting the article: DK and SKL; Critical revision: RZ, MB, AK, DL, DM, SB, AT, RH, and AB; Final approval of the version to be published: SKL
Corresponding author
Ethics declarations
Conflict of interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Khatri, D., Zampolin, R., Behbahani, M. et al. Pediatric brain aneurysms: a review of 1458 brain MR angiograms. Childs Nerv Syst 39, 3249–3254 (2023). https://doi.org/10.1007/s00381-023-05967-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-023-05967-4