Abstract
Objective
To investigate the chronological changes in the clinical presentation and long-term prognosis of pediatric-onset moyamoya disease in our institute over 40 years.
Methods
We evaluated 282 pediatric-onset (≤ 15 years old) moyamoya disease patients who visited our institute from 1981 to 2020 (divided into the former period, 1981–2000, and the latter period, 2001–2020). Differences in the clinical presentation and the long-term outcome were compared between the periods. Multivariate analysis was also performed to reveal the risk factors for poor long-term outcomes.
Results
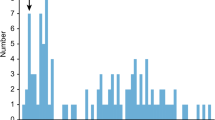
Compared to the former period, the total number of patients, the onset age and both the number of patients with family history and relatively older patients without symptoms or with headache were greater in the latter period (p < 0.05). The number of patients with poor long-term outcomes was significantly lower in the latter period (24.9% vs. 6.7%, p < 0.01). Multivariate analysis revealed that stroke onset, late cerebrovascular events and postoperative complications were independent risk factors for poor long-term outcomes (odds ratio = 31.4, 40.8 and 5.4, respectively).
Conclusions
Over the last 40 years, the number of pediatric moyamoya disease patients has increased, especially in relatively older patients with mild presentation and favorable long-term outcomes. In clinical studies, these chronological changes and the inclusion period of the participants need to be accounted for. Whether the increased diagnostic rate in the recent era has led to a decrease in late cerebrovascular events and favorable outcomes throughout life remains unknown and should be evaluated in the future.



Similar content being viewed by others
Data availability
The full dataset is available from the corresponding author on reasonable request.
References
Tominaga T, Suzuki N, Miyamoto S et al (2012) Guidelines for diagnosis and treatment of moyamoya disease (spontaneous occlusion of the circle of Willis). Neurol Med Chir (Tokyo) 52(5):245–266. https://doi.org/10.2176/nmc.52.245
Shim KW, Park EK, Kim JS, Kim DS (2015) Cognitive outcome of pediatric moyamoya disease. J Korean Neurosurg Soc 57:440–444. https://doi.org/10.3340/jkns.2015.57.6.440
Karasawa J, Touho H, Ohnishi H et al (1992) Long-term follow-up study after extracranial-intracranial bypass surgery for anterior circulation ischemia in childhood moyamoya disease. J Neurosurg 77:84–89. https://doi.org/10.3171/jns.1992.77.1.0084
Zhang D, Huang L, Huang Z et al (2022) Epidemiology of moyamoya disease in China: a nationwide hospital-based study. Lancet Reg Heal - West Pacific 18:100331. https://doi.org/10.1016/j.lanwpc.2021.100331
Ki J, Jy Y, Sc H, JS K (2014) Clinical course of asymptomatic adult moyamoya disease. Cerebrovasc Dis 37:94–101. https://doi.org/10.1159/000356350
Baba T, Houkin K, Kuroda S (2008) Novel epidemiological features of moyamoya disease. J Neurol Neurosurg Psychiatry 79:900–904. https://doi.org/10.1136/JNNP.2007.130666
Kuroda S, Centers C, Center DM et al (2015) Asymptomatic moyamoyadisease: literature review and ongoing AMORE study. Neurol Med Chir (Tokyo) 55:194–198. https://doi.org/10.2176/nmc.ra.2014-0305
Matsushima Y, Maehara T (2004) School class and employment of the moyamoya patients who underwent EDAS more than 10 years previously - related to the acceptance of the disease and long-term QOL -. Nervous System in Children 29(5):368–374
Kim SK, Cho BK, Phi JH (2010) Pediatric moyamoya disease: an analysis of 410 consecutive cases. Ann Neurol 68(1):92–101. https://doi.org/10.1002/ana.21981
Ha EJ, Kim KH, Wang KC (2019) Long-term outcomes of indirect bypass for 629 children with moyamoya disease: longitudinal and cross-sectional analysis. Stroke 50(11):3177–3183. https://doi.org/10.1161/STROKEAHA.119.025609. Epub 2019 Sep 25
Hara S, Nariai T, Inaji M (2021) Imaging pattern and the mechanisms of postoperative infarction after indirect revascularization in patients with moyamoya disease. World Neurosurg 155:e510–e521. https://doi.org/10.1016/j.wneu.2021.08.098. Epub 2021 Aug 28
Houkin K, Nakayama N, Kuroda S et al (2005) Novel magnetic resonance angiography stage grading for moyamoya disease. Cerebrovasc Dis 20:347–354. https://doi.org/10.1159/000087935
Mukawa M, Nariai T, Matsushima Y et al (2012) Long-term follow-up of surgically treated juvenile patients with moyamoya disease. J Neurosurg Pediatr 10:451–456. https://doi.org/10.3171/2012.8.PEDS11539
Van Swieten JC, Koudstaal PJ, Visser MC et al (1988) Interobserver agreement for the assessment of handicap in stroke patients. Stroke 19:604–607. https://doi.org/10.1161/01.STR.19.5.60415
Kanda Y (2013). Investigation of the freely available easy-to-use software’EZR’ for medical statistics. https://doi.org/10.1038/bmt.2012.244
Hara S, Shimizu K, Nariai T et al (2020). De novo renal artery stenosis developed in initially normal renal arteries during the long-term follow-up of patients with moyamoya disease. https://doi.org/10.1016/j.jstrokecerebrovasdis.2020.104786
Yamamoto S, Kashiwazaki D, Uchino H et al (2020) Clinical and radiological features of childhood onset adult moyamoya disease: implication for hemorrhagic stroke. Neurol Med Chir (Tokyo) 60:360–367. https://doi.org/10.2176/NMC.OA.2020-0001
Medical technologies Health at a Glance (2019) OECD Indicators | OECD iLibrary. https://www.oecdilibrary.org/sites/eadc0d9den/index.html?itemId=/content/component/eadc0dd-en. Accessed 8 Oct 2021
Yamashita Y, Murayama S, Okada M et al (2016) The essence of the Japan Radiological Society/Japanese College of Radiology Imaging Guideline. Jpn J Radiol 34:43–79. https://doi.org/10.1007/s11604-015-0499-x
Mukawa M, Nariai T, Matsushima Y, Ohno K (2013) Clinical features of familial juvenile cases of moyamoya disease: analysis of patients treated in a single institute over a 28-year period - Clinical article. J Neurosurg Pediatr 12:175–180. https://doi.org/10.3171/2013.4.PEDS12420
Cho WS, Chung YS, Kim JE et al (2015) The natural clinical course of hemodynamically stable adult moyamoya disease. J Neurosurg 122:82–89. https://doi.org/10.3171/2014.9.JNS132281
Ikeda K, Iwasaki Y, Kashihara H et al (2006) Adult moyamoya disease in the asymptomatic Japanese population. J Clin Neurosci 13:334–338. https://doi.org/10.1016/j.jocn.2005.02.026
Im S-H, Jang D-K, Kim H et al (2021) Long-term mortality in patients with moyamoya angiopathy according to stroke presentation type in South Korea. Acta Neurochir (Wien). https://doi.org/10.1007/s00701-021-04959-0
Lee J, Kim SK, Kang HG (2019) High prevalence of systemic hypertension in pediatric patients with moyamoya disease years after surgical treatment. J Neurosurg Pediatr 8:1–7. https://doi.org/10.3171/2019.9.PEDS1986. Epub ahead of print
Funaki T, Takahashi JC, Miyamoto S (2018) Late cerebrovascular events and social outcome after adolescence: long-term outcome of pediatric moyamoya disease. Neurol Med Chir (Tokyo) 58:240–246. https://doi.org/10.2176/nmc.ra.2018-0026. (Epub 2018 May 21)
Funding
This work was supported by Grants-in-Aid for Scientific Research “KAKENHI,” the Japan Society for the Promotion of Science, Grant #19K18406, given to Shoko Hara.
Author information
Authors and Affiliations
Contributions
Conceptualization: Shoko Hara and Tadashi Nariai; Methodology: Mai Fujioka, Maki Mukawa, and Shoko Hara; Formal analysis and investigation: Mai Fujioka, Maki Mukawa, Jun Karakama, and Shoko Hara; Writing—original draft preparation: Mai Fujioka; Writing—review and editing: Shoko Hara, Maki Mukawa, Motoki Inaji, Yoji Tanaka, Tadashi Nariai, and Taketoshi Maehara; Funding acquisition: Shoko Hara; Resources: Maki Mukawa, Shoko Hara, Motoki Inaji, Yoji Tanaka, Tadashi Nariai, and Taketoshi Maehara; Supervision: Tadashi Nariai and Taketoshi Maehara.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the ethical committee of the local institutional review board (M2000-1331), and informed consent was obtained from all of the participants.
Consent for publication
Consent for publication was obtained from all of the participants.
Conflict of interest
No conflict of interest exists.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fujioka, M., Hara, S., Mukawa, M. et al. Changes in the clinical spectrum of pediatric moyamoya disease over 40 years. Childs Nerv Syst 39, 1215–1223 (2023). https://doi.org/10.1007/s00381-023-05852-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-023-05852-0