Abstract
Background
In 2001, the National Academy of Medicine, formerly known as the Institute of Medicine (IOM), published their seminal work, Crossing the Quality Chasm: A New Health System for the 21st Century. In this work, the authors called for improved safety, effectiveness, patient-centeredness, timeliness, efficiency, and equity in the United States’ healthcare system. Two decades after the publication of this work, healthcare costs continue to rise, but outcomes lag other nations. The objective of this narrative review is to describe research efforts in pediatric neurosurgery with respect to the six quality aims proposed by the IOM, and highlight additional research opportunities.
Methods
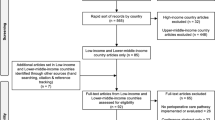
PubMed, Google Scholar, and EBSCOhost were queried to identify studies in pediatric neurosurgery that have addressed the aims proposed by the IOM. Studies were summarized and synthesized to develop a set of research opportunities to advance quality of care.
Results
Twenty-three studies were reviewed which focused on the six quality aims proposed by the IOM. Out of these studies, five research opportunities emerged: (1) To examine performance of tools of care, (2) To understand processes surrounding care delivery, (3) To conduct cost-effectiveness analyses for a broader range of neurosurgical conditions, (4) To identify barriers driving healthcare disparities, and (5) To understand patients’ and caregivers’ experiences receiving care, and subsequently develop tools and programs to address their needs and preferences.
Conclusion
There is a growing body of literature examining quality in pediatric neurosurgical care across all aims proposed by the IOM. However, there remains important gaps in the literature that, if addressed, will advance the quality of pediatric neurosurgical care delivery.
Similar content being viewed by others
Availability of data and materials
N/A.
References
Hogan H, Healey F, Neale G et al (2012) Preventable deaths due to problems in care in English acute hospitals: a retrospective case record review study. BMJ Qual Saf 21:737–745. https://doi.org/10.1136/bmjqs-2011-001159
Hogan H, Zipfel R, Neuburger J et al (2015) Avoidability of hospital deaths and association with hospital-wide mortality ratios: retrospective case record review and regression analysis. BMJ 351:h3239. https://doi.org/10.1136/bmj.h3239
Manaseki-Holland S, Lilford RJ, Bishop JRB et al (2017) Reviewing deaths in British and US hospitals: a study of two scales for assessing preventability. BMJ Qual Saf 26:408–416. https://doi.org/10.1136/bmjqs-2015-004849
Khan A, Coffey M, Litterer KP et al (2017) Families as partners in hospital error and adverse event surveillance. JAMA Pediatr 171:372–381. https://doi.org/10.1001/jamapediatrics.2016.4812
Proctor ML, Pastore J, Gerstle JT et al (2003) Incidence of medical error and adverse outcomes on a pediatric general surgery service. J Pediatr Surg 38:1361–1365. https://doi.org/10.1016/S0022-3468(03)00396-8
U.S. Centers for Medicare & Medicaid Services. National Health Expenditures 2020 Highlights. https://www.cms.gov/files/document/highlights.pdf
Mirror, Mirror (2021) Reflecting poorly. 2021. https://doi.org/10.26099/01dv-h208
Rolston JD, Zygourakis CC, Han SJ et al (2014) Medical errors in neurosurgery. Surg Neurol Int 5:S435–S440. https://doi.org/10.4103/2152-7806.142777
Institute of Medicine (US) Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington (DC): National Academies Press (US); 2001. Available from: https://www.ncbi.nlm.nih.gov/books/NBK222274/https://doi.org/10.17226/10027. Accessed 7 Sep 2021
Berwick DM, Nolan TW, Whittington J (2008) The triple aim: care, health, and cost. Health Aff (Millwood) 27:759–769. https://doi.org/10.1377/hlthaff.27.3.759
Bodenheimer T, Sinsky C (2014) From triple to quadruple aim: care of the patient requires care of the provider. Ann Fam Med 12:573–576. https://doi.org/10.1370/afm.1713
Donabedian A (1988) The quality of care. How can it be assessed? JAMA 260:1743–8. https://doi.org/10.1001/jama.260.12.1743
World Health Organization. Safe surgery. Safe Surg. https://www.who.int/teams/integrated-healthservices/patient-safety/research/safe-surgery (Accessed 21 Feb 2022)
Neurosurgical checklists a review in: Neurosurgical Focus Volume 33 Issue 5 (2012) Journals. https://thejns-org.stanford.idm.oclc.org/focus/view/journals/neurosurg-focus/33/5/article-pE2.xml. Accessed 21 Feb 2022
Fargen KM, Velat GJ, Lawson MF et al (2013) Enhanced staff communication and reduced near-miss errors with a neurointerventional procedural checklist. J NeuroInterventional Surg 5:497–500. https://doi.org/10.1136/neurintsurg-2012-010430
Lee RP, Venable GT, Vaughn BN et al (2018) The impact of a pediatric shunt surgery checklist on infection rate at a single institution. Neurosurgery 83:508–520. https://doi.org/10.1093/neuros/nyx478
Parker SL, McGirt MJ, Murphy JA et al (2015) Cost savings associated with antibiotic-impregnated shunt catheters in the treatment of adult and pediatric hydrocephalus. World Neurosurg 83:382–386. https://doi.org/10.1016/j.wneu.2014.06.010
Mohole J, Ho AL, Cannon JGD et al (2019) Topical vancomycin for surgical prophylaxis in pediatric craniofacial surgeries. J Craniofac Surg 30:2163–2167. https://doi.org/10.1097/SCS.0000000000005708
Cannon JGD, Ho AL, Mohole J et al (2019) Topical vancomycin for surgical prophylaxis in non-instrumented pediatric spinal surgeries. Childs Nerv Syst ChNS Off J Int Soc Pediatr Neurosurg 35:107–111. https://doi.org/10.1007/s00381-018-3881-z
Gonda DD, Fridley J, Ryan SL et al (2015) The safety and efficacy of use of low-molecular-weight heparin in pediatric neurosurgical patients. J Neurosurg Pediatr 16:329–334. https://doi.org/10.3171/2015.1.PEDS14489
Vadivelu S, Sivaganesan A, Patel AJ et al (2014) Practice trends in the utilization of intraoperative neurophysiological monitoring in pediatric neurosurgery as a function of complication rate, and patient-, surgeon-, and procedure-related factors. World Neurosurg 81:617–623. https://doi.org/10.1016/j.wneu.2013.11.010
Giordano M, Samii A, McLean ACL et al (2017) Intraoperative magnetic resonance imaging in pediatric neurosurgery: safety and utility. J Neurosurg Pediatr 19:77–84. https://doi.org/10.3171/2016.8.PEDS15708
Okubo Y, Fallah A, Hayakawa I et al (2020) Trends in hospitalization and readmission for pediatric epilepsy and underutilization of epilepsy surgery in the United States. Seizure 80:263–269. https://doi.org/10.1016/j.seizure.2020.05.013
Sacino M, Huang SS, Alexander H et al (2020) An initial cost-effectiveness analysis of magnetic resonance-guided laser interstitial thermal therapy in pediatric epilepsy surgery. Pediatr Neurosurg 55:141–148. https://doi.org/10.1159/000509329
Sacino MF, Huang SS, Keating RF et al (2018) An initial cost-effectiveness analysis of intraoperative magnetic resonance imaging (iMRI) in pediatric epilepsy surgery. Childs Nerv Syst 34:495–502. https://doi.org/10.1007/s00381-017-3658-9
Lim J, Tang AR, Liles C et al (2018) The cost of hydrocephalus: a cost-effectiveness model for evaluating surgical techniques. J Neurosurg Pediatr 23:109–118. https://doi.org/10.3171/2018.6.PEDS17654
Liles C, Dallas J, Hale AT et al (2019) The economic impact of open versus endoscope-assisted craniosynostosis surgery. J Neurosurg Pediatr 1–8. https://doi.org/10.3171/2019.4.PEDS18586
Graves JM, Kannan N, Mink RB et al (2016) Guideline adherence and hospital costs in pediatric severe traumatic brain injury*. Pediatr Crit Care Med 17:438–443. https://doi.org/10.1097/PCC.0000000000000698
Attenello FJ, Ng A, Wen T et al (2015) Racial and socioeconomic disparities in outcomes following pediatric cerebrospinal fluid shunt procedures. J Neurosurg Pediatr 15:560–566. https://doi.org/10.3171/2014.11.PEDS14451
Walker CT, Stone JJ, Jain M et al (2014) The effects of socioeconomic status and race on pediatric neurosurgical shunting. Childs Nerv Syst ChNS Off J Int Soc Pediatr Neurosurg 30:117–122. https://doi.org/10.1007/s00381-013-2206-5
Vedantam A, Pan I-W, Staggers KA et al (2018) Thirty-day outcomes in pediatric epilepsy surgery. Childs Nerv Syst 34:487–494. https://doi.org/10.1007/s00381-017-3639-z
Shweikeh F, Foulad D, Nuño M et al (2016) Differences in surgical outcomes for patients with craniosynostosis in the US: impact of socioeconomic variables and race. J Neurosurg Pediatr 17:27–33. https://doi.org/10.3171/2015.4.PEDS14342
Lin Y, Pan I-W, Harris DA et al (2015) The impact of insurance, race, and ethnicity on age at surgical intervention among children with nonsyndromic craniosynostosis. J Pediatr 166:1289–1296. https://doi.org/10.1016/j.jpeds.2015.02.007
Jackson HN, Gadgil N, Pan I-W et al (2020) Sociodemographic factors in pediatric epilepsy surgery. Pediatr Neurol 107:71–76. https://doi.org/10.1016/j.pediatrneurol.2019.09.002
James HE (2016) Pediatric neurosurgery telemedicine clinics: a model to provide care to geographically underserved areas of the United States and its territories. J Neurosurg Pediatr 18:753–757. https://doi.org/10.3171/2016.6.PEDS16202
Hayward K, Han SH, Simko A et al (2019) Socioeconomic patient benefits of a pediatric neurosurgery telemedicine clinic. J Neurosurg Pediatr 25:204–208. https://doi.org/10.3171/2019.8.PEDS1925
Simko AP, Hudak ML, Han SH et al (2022) Economic analysis of a pediatric neurosurgery telemedicine clinic. J Neurosurg Pediatr 1:1–6. https://doi.org/10.3171/2021.12.PEDS21403
Waseem H, Mazzamurro RS, Fisher AH et al (2018) Parental satisfaction with being present in the operating room during the induction of anesthesia prior to pediatric neurosurgical intervention: a qualitative analysis. J Neurosurg Pediatr 21:528–534. https://doi.org/10.3171/2017.10.PEDS17261
Thomas Craig KJ, McKillop MM, Huang HT et al (2020) U.S. hospital performance methodologies: a scoping review to identify opportunities for crossing the quality chasm. BMC Health Serv Res 20:640. https://doi.org/10.1186/s12913-020-05503-z
Aveling E-L, Stone J, Sundt T et al (2018) Factors influencing team behaviors in surgery: a qualitative study to inform teamwork interventions. Ann Thorac Surg 106:115–120. https://doi.org/10.1016/j.athoracsur.2017.12.045
Molina G, Singal R, Haynes AB et al (2017) Perception of safety of surgical practice among healthcare professionals who work in an operating room in ambulatory surgery centers in the United States: a retrospective analysis of survey data. Perioper Care Oper Room Manag 8:12–18. https://doi.org/10.1016/j.pcorm.2017.07.002
Savchuk S, Jin MC, Choi S et al (2021) Incorporating patient-centered quality-of-life measures for outcome assessment after Chiari malformation type I decompression in a pediatric population: a pilot study. J Neurosurg Pediatr 29:200–207. https://doi.org/10.3171/2021.8.PEDS21228
Toomey SL, Zaslavsky AM, Elliott MN et al (2015) The development of a pediatric inpatient experience of care measure: child HCAHPS®. Pediatrics 136:360–369. https://doi.org/10.1542/peds.2015-0966
Funding
This publication was generously supported by the Stanford Maternal and Child Health Research Institute Structural Racism, Social Injustice and Health Disparities Program as well as the Stanford University Medical Scholars Program.
Author information
Authors and Affiliations
Contributions
GRC and LMP contributed to the conceptualization of this manuscript. GRC drafted the manuscript. AW, JKR, and LMP contributed to interpretation of findings and critically revised the manuscript for intellectual content. All authors approved of the submitted version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
N/A.
Consent for publication
Granted by all authors.
Conflict of interest
N/A.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Previous presentations: None.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ruiz Colón, G.D., Wu, A., Ratliff, J.K. et al. Quality and patient safety research in pediatric neurosurgery: a review. Childs Nerv Syst 39, 1147–1158 (2023). https://doi.org/10.1007/s00381-022-05821-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-022-05821-z