Abstract
Purpose
Hyponatremia after craniotomy can be associated with increased morbidity. However, the incidence of and factors associated with post-craniotomy hyponatremia in children are not known.
Methods
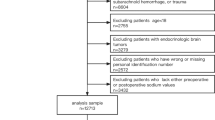
We performed a retrospective cohort study of patients aged 0–21 years who underwent craniotomy in 2017–2019 at a single center to determine the incidence of and to identify risk factors for hyponatremia after craniotomy. Indications for craniotomy included tumors (excluding craniopharyngioma), epilepsy, intracranial infection, trauma, craniofacial, suboccipital decompression for the treatment of Chiari malformation, and cerebrovascular disease. Hyponatremia was defined as a serum sodium level ≤ 135 mEq/L any time during the postoperative hospital stay. Statistical significance was defined a priori at p < 0.05.
Results
Postoperative hyponatremia occurred in 61 (25%) of 240 children. On univariate analysis, hyponatremia was associated with younger age (8.5 vs 6.3 years, p = 0.01), use of preoperative anti-epileptic drugs (p = 0.02), need for blood transfusion (p = 0.02), government/private insurance (p = 0.04), and pre-existing hydrocephalus, defined as the requirement for permanent cerebrospinal fluid (CSF) diversion (p = 0.04). On multivariate analysis, only hydrocephalus (OR 2.95, 95% CI 1.03–8.40) remained statistically significant. Hyponatremia most occurred on the first postoperative day, with normonatremia achieved in a median of 14 (IQR 9.8–24.3) h. Hyponatremia was significantly associated with longer length of stay (median 8 vs 3 days, p < 0.01).
Conclusion
Hyponatremia was present in 25% of children after craniotomy. Preoperative hydrocephalus as an independent risk factor for hyponatremia after craniotomy.
Similar content being viewed by others
Data availability
Data will be made available after contacting the corresponding author. The appropriate regulatory steps have been taken.
Abbreviations
- BUN:
-
Blood urea nitrogen
- CSW:
-
Cerebral salt wasting
- CSF:
-
Cerebrospinal fluid
- EDAS:
-
Encephaloduraateriosynagiosis
- ETV:
-
Endoscopic third ventriculostomy
- EVD:
-
External ventricular drain
- ICU:
-
Intensive care unit
- IQR:
-
Inter-quantile range
- OR:
-
Odds ratio
- SIADH:
-
Syndrome of Inappropriate secretion of Anti-Diuretic Hormone
- WHO:
-
World Health Organization
References
Wise BL (1960) Hyponatremia following craniotomy. Arch Neurol 2:391–398. https://doi.org/10.1001/archneur.1960.03840100029005
Belzer JS, Williams CN, Riva-Cambrin J, Presson AP, Bratton SL (2014) Timing, duration, and severity of hyponatremia following pediatric brain tumor surgery*. Pediatr Crit Care Med 15:456–463. https://doi.org/10.1097/pcc.0000000000000154
Williams C, Simon TD, Riva-Cambrin J, Bratton SL (2012) Hyponatremia with intracranial malignant tumor resection in children. J Neurosurg Pediatr 9:524–529. https://doi.org/10.3171/2012.1.Peds11465
Williams CN, Belzer JS, Riva-Cambrin J, Presson AP, Bratton SL (2014) The incidence of postoperative hyponatremia and associated neurological sequelae in children with intracranial neoplasms. J Neurosurg Pediatr 13:283–290. https://doi.org/10.3171/2013.12.Peds13364
Williams CN, Riva-Cambrin J, Bratton SL (2016) Etiology of postoperative hyponatremia following pediatric intracranial tumor surgery. J Neurosurg Pediatr 17:303–309. https://doi.org/10.3171/2015.7.Peds15277
Williams CN, Riva-Cambrin J, Presson AP, Bratton SL (2015) Hyponatremia and poor cognitive outcome following pediatric brain tumor surgery. J Neurosurg Pediatr 15:480–487. https://doi.org/10.3171/2014.10.Peds14368
Levine JP, Stelnicki E, Weiner HL, Bradley JP, McCarthy JG (2001) Hyponatremia in the postoperative craniofacial pediatric patient population: a connection to cerebral salt wasting syndrome and management of the disorder. Plast Reconstr Surg 108:1501–1508. https://doi.org/10.1097/00006534-200111000-00009
Prete A, Corsello SM, Salvatori R (2017) Current best practice in the management of patients after pituitary surgery. Ther Adv Endocrinol Metab 8:33–48. https://doi.org/10.1177/2042018816687240
Hardesty DA, Kilbaugh TJ, Storm PB (2012) Cerebral salt wasting syndrome in post-operative pediatric brain tumor patients. Neurocrit Care 17:382–387. https://doi.org/10.1007/s12028-011-9618-4
Kinik ST, Kandemir N, Baykan A, Akalan N, Yordam N (2001) Fludrocortisone treatment in a child with severe cerebral salt wasting. Pediatr Neurosurg 35:216–219. https://doi.org/10.1159/000050424
Cui H et al (2019) Inappropriate antidiuretic hormone secretion and cerebral salt-wasting syndromes in neurological patients. Front Neurosci 13:1170. https://doi.org/10.3389/fnins.2019.01170
Moritz ML, Ayus JC (2010) New aspects in the pathogenesis, prevention, and treatment of hyponatremic encephalopathy in children. Pediatr Nephrol 25:1225–1238. https://doi.org/10.1007/s00467-009-1323-6
Oh GJ, Sutherland SM (2016) Perioperative fluid management and postoperative hyponatremia in children. Pediatr Nephrol 31:53–60. https://doi.org/10.1007/s00467-015-3081-y
Acknowledgements
The authors would like the thank the Faculty and Staff within the Division of Pediatric Neurosurgery at Children’s of Alabama for their support of this work.
Author information
Authors and Affiliations
Contributions
Olivia Keating, Andrew T. Hale, Anastasia A. Smith, and Victoria Jimenez collected data. Olivia Keating, Andrew T. Hale, and Brandon G. Rocque performed statistical analysis. Olivia Keating wrote the first draft of the manuscript. The final manuscript was approved by all authors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Institutional Review Board (IRB) approval and appropriate consent (where applicable) was obtained under the governance of the University of Alabama at Birmingham.
Consent for publication
Consent (where applicable) was obtained for publication of these results.
Conflict of interest
The authors declare that no competing interests exist as related to this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Keating, O., Hale, A.T., Smith, A.A. et al. Hyponatremia after craniotomy in children: a single-institution review. Childs Nerv Syst 39, 617–623 (2023). https://doi.org/10.1007/s00381-022-05729-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-022-05729-8