Abstract
Purpose
Pediatric pituitary adenomas (pPAs) are uncommon. Thus, their presentation and outcomes after treatment are less well-understood than those of pituitary adenomas in adulthood (aPAs).
Methods
A retrospective chart review was conducted for all patients who underwent endoscopic endonasal transsphenoidal surgery (EETS) for pPA at NewYork-Presbyterian Hospital/Weill Cornell Medicine (NYP/WCM) from 2005–2020. Eleven patients were identified, and information pertaining to age, sex, adenoma characteristics, procedural details, and outcomes was reviewed. A systematic review of the literature was also performed to compare outcomes of EETS versus microscopic endonasal transsphenoidal surgery (METS) for pPA.
Results
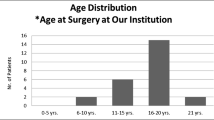
From 2005–2020, 11 patients underwent EETS for pPA at NYP/WCM. Mean age at operation was 14.9 ± 2.7 years, and 5 patients (45.5%) were male. 10 adenomas (90.9%) were hormone-producing. Of the functional adenomas, 8 (80.0%) were PRL-secreting and 2 (20.0%) were GH-secreting. Maximum adenoma diameter (MAD) ranged from 1.2–5.1 cm, with a median of 1.55 cm. Cavernous sinus invasion (CSI) occurred in 2 patients with macroprolactinoma. Gross total resection (GTR) was achieved in 10 (90.9%). Biochemical remission occurred in 5/10 (50.0%). Post-operative complications were documented in 8 cases (72.7%) and included diabetes insipidus, hypopituitarism, sinusitis, weight gain, cerebrospinal fluid leak, meningitis, and hydrocephalus. Systematic literature review of 105 microscopic and 175 endoscopic cases revealed high frequency of hormone-producing tumors (83.6%) and similar rates of GTR (82.4% vs 85.1%) and biochemical cure (75.8% vs 64.3%).
Conclusions
pPAs are more likely to be hormone producing and may be more aggressive and difficult to cure than aPAs. EETS is an effective treatment, although complication rates may be higher than in adult populations.

Similar content being viewed by others
References
Perry A, Graffeo CS, Marcellino C, Pollock BE, Wetjen NM, Meyer FB (2018) Pediatric Pituitary Adenoma: Case Series, Review of the Literature, and a Skull Base Treatment Paradigm. J Neurol Surgery Part B Skull Base. Published Online. https://doi.org/10.1055/s-0038-1625984
Walz PC, Drapeau A, Shaikhouni A et al (2019) Pediatric pituitary adenomas. Child’s Nerv Syst. Published online. https://doi.org/10.1007/s00381-019-04293-y
Marino AC, Taylor DG, Desai B, Jane JA (2019) Surgery for Pediatric Pituitary Adenomas. Neurosurg Clin N Am. Published online. https://doi.org/10.1016/j.nec.2019.05.008
Wang H, Wang R, Hu T et al (2020) Nonfunctioning pituitary adenomas in pediatric and adolescent patients: a clinical analysis of a series of 14 patients. J Neurooncol. Published online. https://doi.org/10.1007/s11060-020-03512-w
Broersen LHA, Biermasz NR, van Furth WR et al (2018) Endoscopic vs. microscopic transsphenoidal surgery for Cushing’s disease: a systematic review and meta-analysis. Pituitary. Published Online. https://doi.org/10.1007/s11102-018-0893-3
Komotar RJ, Starke RM, Raper DMS, Anand VK, Schwartz TH (2012) Endoscopic endonasal compared with microscopic transsphenoidal and open transcranial resection of giant pituitary adenomas. Pituitary. Published online. https://doi.org/10.1007/s11102-011-0359-3
Møller MW, Andersen MS, Glintborg D et al (2020) Endoscopic vs. microscopic transsphenoidal pituitary surgery: a single centre study. Sci Rep. Published online. https://doi.org/10.1038/s41598-020-78823-z
Knosp E, Steiner E, Kitz K, Matula C (1993) Pituitary adenomas with invasion of the cavernous sinus space: A magnetic resonance imaging classification compared with surgical findings. Neurosurgery. Published online. https://doi.org/10.1227/00006123-199310000-00008
Hofstetter CP, Mannaa RH, Mubita L et al (2010) Endoscopic endonasal transsphenoidal surgery for growth hormone-secreting pituitary adenomas. Neurosurg Focus. Published online. https://doi.org/10.3171/2010.7.FOCUS10173
Mascarenhas L, Moshel YA, Bayad F et al (2014) The Transplanum Transtuberculum Approaches for Suprasellar and Sellar-Suprasellar Lesions: Avoidance of Cerebrospinal Fluid Leak and Lessons Learned. World Neurosurg. Published online. https://doi.org/10.1016/j.wneu.2013.02.032
Marcus HJ, Khan DZ, Borg A et al (2021) Pituitary society expert Delphi consensus: operative workflow in endoscopic transsphenoidal pituitary adenoma resection. Pituitary. Published online. https://doi.org/10.1007/s11102-021-01162-3
Woodworth GF, Patel KS, Shin B et al (2014) Surgical outcomes using a medial-to-lateral endonasal endoscopic approach to pituitary adenomas invading the cavernous sinus: Clinical article. J Neurosurg. Published online. https://doi.org/10.3171/2014.1.JNS131228
Patel KS, Komotar RJ, Szentirmai O et al (2013) Case-specific protocol to reduce cerebrospinal fluid leakage after endonasal endoscopic surgery. J Neurosurg. Published online. https://doi.org/10.3171/2013.4.JNS13124
Kumar Upadhyay A, Kumar V, Kumar Gupta A, Rastogi M, Husain M (2020) Microscopic Trans-sphenoidal surgery in paediatric pituitary adenoma: An institutional experience. IP Indian J Neurosci. Published Online. https://doi.org/10.18231/j.ijn.2020.004
Mindermann T, Wilson CB (1995) Pediatric pituitary adenomas. Neurosurgery. Published online. https://doi.org/10.1227/00006123-199502000-00004
Partington MD, Davis DH, Laws ER, Scheithauer BW (1994) Pituitary adenomas in childhood and adolescence. Results of transsphenoidal surgery. J Neurosurg. Published Online. https://doi.org/10.3171/jns.1994.80.2.0209
Bălinişteanu B, Cîmpean AM, Ceauşu AR, Corlan AS, Melnic E, Raica M (2017) High Ki-67 expression is associated with prolactin secreting pituitary adenomas. Bosn J Basic Med Sci. Published Online. https://doi.org/10.17305/bjbms.2017.1750
Sadeghipour A, Mahouzi L, Salem MM et al (2017) Ki67 labeling correlated with invasion but not with recurrence. Appl Immunohistochem Mol Morphol. Published online. https://doi.org/10.1097/PAI.0000000000000303
Hannah-Shmouni F, Stratakis CA (2018) An update on the genetics of benign pituitary adenomas in children and adolescents. Curr Opin Endocr Metab Res. Published Online. https://doi.org/10.1016/j.coemr.2018.04.002
Tatsi C, Stratakis CA (2019) The Genetics of Pituitary Adenomas. J Clin Med. Published online. https://doi.org/10.3390/jcm9010030
Ammirati M, Wei L, Ciric I (2013) Short-term outcome of endoscopic versus microscopic pituitary adenoma surgery: A systematic review and meta-analysis. J Neurol Neurosurg Psychiatry. Published online. https://doi.org/10.1136/jnnp-2012-303194
Li A, Liu W, Cao P, Zheng Y, Bu Z, Zhou T (2017) Endoscopic Versus Microscopic Transsphenoidal Surgery in the Treatment of Pituitary Adenoma: A Systematic Review and Meta-Analysis. World Neurosurg. Published online. https://doi.org/10.1016/j.wneu.2017.01.022
Gao Y, Zhong C, Wang Y et al (2014) Endoscopic versus microscopic transsphenoidal pituitary adenoma surgery: A meta-analysis. World J Surg Oncol. Published online. https://doi.org/10.1186/1477-7819-12-94
Razak AA, Horridge M, Connolly DJ et al (2013) Comparison of endoscopic and microscopic trans-sphenoidal pituitary surgery: Early results in a single centre. Br J Neurosurg. Published online. https://doi.org/10.3109/02688697.2012.703353
Lenzi J, Lapadula G, D’Amico T et al (2015) Evaluation of trans-sphenoidal surgery in pituitary GH-secreting micro- and macroadenomas: A comparison between microsurgical and endoscopic approach. J Neurosurg Sci. Published online
Cheng RX, Tian HL, Gao WW, Li ZQ (2011) A comparison between endoscopic transsphenoidal surgery and traditional trans-sphenoidal microsurgery for functioning pituitary adenomas. J Int Med Res. Published online. https://doi.org/10.1177/147323001103900545
Kenan K, İhsan A, Dilek O, Burak C, Gurkan K, Savas C (2006) The learning curve in endoscopic pituitary surgery and our experience. Neurosurg Rev. Published online. https://doi.org/10.1007/s10143-006-0033-9
Jane JA, Starke RM, Elzoghby MA et al (2011) Endoscopic transsphenoidal surgery for acromegaly: Remission using modern criteria, complications, and predictors of outcome. J Clin Endocrinol Metab. Published online. https://doi.org/10.1210/jc.2011-0554
Campbell PG, Kenning E, Andrews DW, Yadla S, Rosen M, Evans JJ (2010) Outcomes after a purely endoscopic transsphenoidal resection of growth hormone-secreting pituitary adenomas. Neurosurg Focus. Published online. https://doi.org/10.3171/2010.7.FOCUS10153
Tampourlou M, Trifanescu R, Paluzzi A, Ahmed SK, Karavitaki N (2016) Therapy of endocrine disease - Surgery in microprolactinomas: Effectiveness and risks based on contemporary literature. Eur J Endocrinol. Published online. https://doi.org/10.1530/EJE-16-0087
Primeau V, Raftopoulos C, Maiter D (2012) Outcomes of transsphenoidal surgery in prolactinomas: Improvement of hormonal control in dopamine agonist-resistant patients. Eur J Endocrinol. Published online. https://doi.org/10.1530/EJE-11-1000
Agam MS, Wedemeyer MA, Wrobel B, Weiss MH, Carmichael JD, Zada G (2019) Complications associated with microscopic and endoscopic transsphenoidal pituitary surgery: Experience of 1153 consecutive cases treated at a single tertiary care pituitary center. J Neurosurg. Published online. https://doi.org/10.3171/2017.12.JNS172318
Younus I, Gerges MM, Uribe-Cardenas R et al (2020) The slope of the learning curve in 600 consecutive endoscopic transsphenoidal pituitary surgeries. Acta Neurochir (Wien). Published Online. https://doi.org/10.1007/s00701-020-04471-x
Dubois S, Guyétant S, Menei P et al (2007) Relevance of Ki-67 and prognostic factors for recurrence/progression of gonadotropic adenomas after first surgery. Eur J Endocrinol. Published online. https://doi.org/10.1530/EJE-07-0099
Yarman S, Kurtulmus N, Canbolat A, Bayindir C, Bilgic B, Ince N (2010) Expression of Ki-67, p53 and vascular endothelial growth factor (VEGF) concomitantly in growth hormone-secreting pituitary adenomas; which one has a role in tumor behavior?. Neuroendocrinol Lett. Published online
Gandour-Edwards R, Kapadia SB, Janecka IP, Martinez AJ, Barnes L (1995) Biologic markers of invasive pituitary adenomas involving the sphenoid sinus. Mod Pathol. Published online
Jiao W, Huang Y, Sun W, Lei T (2017) Microscopic Transnasal Transsphenoidal Surgery for Pediatric Pituitary Adenomas. J Craniofac Surg 28(4):1010–1012. https://doi.org/10.1097/SCS.0000000000003632
Tarapore PE, Sughrue ME, Blevins L et al (2011) Microscopic endonasal transsphenoidal pituitary adenomectomy in the pediatric population. J Neurosurg Pediatr 7(5):501–509. https://doi.org/10.3171/2011.2.PEDS10278
Gazioglu N, Canaz H, Camlar M, Tanrıöver N, Kocer N, Islak C, Evliyaoglu O, Ercan O (2019) Neurosurgical treatment of Cushing disease in pediatric patients: case series and review of literature. Child Nerv Sys. https://doi.org/10.1007/s00381-018-4013-5
Chivukula S, Koutourousiou M, Snyderman CH et al (2013) Endoscopic endonasal skull base surgery in the pediatric population. J Neurosurg Pediatr 11(3):227–241. https://doi.org/10.3171/2012.10.PEDS12160
Giovannetti F, Mussa F, Priore P et al (2018) Endoscopic endonasal skull base surgery in pediatric patients. A single center experience. J Craniomaxillofac Surg 46(12):2017–2021. https://doi.org/10.1016/j.jcms.2018.09.013
Kassam A, Thomas AJ, Snyderman C et al (2007) Fully endoscopic expanded endonasal approach treating skull base lesions in pediatric patients. J Neurosurg 106(2 Suppl):75–86. https://doi.org/10.3171/ped.2007.106.2.75
Kim YH, Lee JY, Phi JH et al (2019) Endoscopic endonasal skull base surgery for pediatric brain tumors. Childs Nerv Syst 35(11):2081–2090. https://doi.org/10.1007/s00381-019-04335-5
Koumas C, Laibangyang A, Barron SL et al (2019) Outcomes following endoscopic endonasal resection of sellar and uprasellar lesions in pediatric patients. Childs Nerv Syst 35(11):2099–2105. https://doi.org/10.1007/s00381-019-04258-1
Locatelli D, Massimi L, Rigante M et al (2010) Endoscopic endonasal transsphenoidal surgery for sellar tumors in children. Int J Pediatr Otorhinolaryngol 74(11):1298–1302. https://doi.org/10.1016/j.ijporl.2010.08.009
Phi JH, Kim YH, Kim JH, Kim DG (2016) Clinical and Anatomic Features of Supraglandular Pituitary Adenomas. World Neurosurg 92:241–248. https://doi.org/10.1016/j.wneu.2016.03.094
Quon JL, Kim LH, Hwang PH et al (2019) Transnasal endoscopic approach for pediatric skull base lesions: a case series [published online ahead of print, 2019 Jun 14]. J Neurosurg Pediatr 1–12. https://doi.org/10.3171/2019.4.PEDS18693
Storr HL, Drake WM, Evanson J et al (2014) Endonasal endoscopic transsphenoidal pituitary surgery: early experience and outcome in paediatric Cushing’s disease. Clin Endocrinol (Oxf) 80(2):270–276. https://doi.org/10.1111/cen.12275\
Zhan R, Xu G, Wiebe TM, Li X (2015) Surgical outcomes of the endoscopic transsphenoidal route to pituitary tumours in paediatric patients >10 years of age: 5 years of experience at a single institute. Arch Dis Child 100(8):774–778. https://doi.org/10.1136/archdischild-2015-308365
Zhan R, Xin T, Li X et al (2015) Endonasal Endoscopic Transsphenoidal Approach to Lesions of the Sellar Region in Pediatric Patients. J Craniofac Surg 26(6):1818–1822. https://doi.org/10.1097/SCS.0000000000001946
Davide, Locatelli Pierlorenzo, Veiceschi Paolo, Castelnuovo Necmettin, Tanriover Olcay, Evliyaoglu Huseyin, Canaz Doga, Ugurlar Nurperi, Gazioglu (2019) Transsphenoidal surgery for pituitary adenomas in pediatric patients: a multicentric retrospective study. Child's Nervous System 35(11) 2119-2126. https://doi.org/10.1007/s00381-019-04179-z
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
On behalf of all authors, the corresponding author states that there are no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kelly, A.P., Greenfield, J.P., Dobri, G.A. et al. Pediatric pituitary adenomas are more aggressive, more likely to be hormone producing and are more difficult to cure than adult pituitary adenomas: case series and systematic literature review. Childs Nerv Syst 38, 729–738 (2022). https://doi.org/10.1007/s00381-022-05445-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-022-05445-3