Abstract
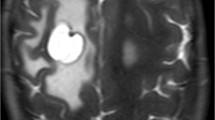
We report a 22-year-old man who had abdominal shunt tube migration into colon. He was diagnosed with pilocytic astrocytoma at optic-chiasm to hypothalamus at age of 7, and treated by resection, chemotherapy, and irradiation. He developed hydrocephalus and had multiple ventriculo-peritoneal shunt surgery. At age of 19, he fell in coma due to the subarachnoid and intra-ventricular hemorrhage due to the aneurysm rupture. The ventricle tube was removed, leaving the shunt valve and abdominal tube. The new shunt system was reconstructed at the contralateral side. He was at bed rest after this episode. At age of 20, he had high fever unable to control with antibiotics. The abdominal computed tomogram showed the shunt tube migration in the descending colon. The tube was removed under laparoscopy, and the inflammation was cured. The abandoned peritoneal shunt tube should be removed in patients with high tube migration risks.



Similar content being viewed by others
References
Kutty RK, Sreemathyamma SB, Sivanandapanicker JL, Asher P, Peethambaran A (2019) A shunt lsot in the mists of time. Childs Nerv Syst 35:2427–2430
Riccardello GJ Jr, Barr LK, Bassani L (2016) Bowel perforation presenting with acute abdominal pain and subcutaneous emphysema in a 14-year-old girl with an abandoned distal peritoneal shunt catheter: case repot. J Neurosurg Pediatr 18:325–328
Vinchon M, Baroncini M, Laurent T, Patrick D (2006) Bowel perforation caused by peritoneal shunt catheters: diagnosis and treatment. Neurosurgery 58: ONS76–82; discussion ONS76–82
Adib SD, Lescan M, Renovanz M, Schuhmann MU, Trakolis L, Bongers M, Tatagiba M, Dobele A, Grozinger G (2020) Intracardial catheter migration of a ventriculoperitoneal shunt: pathophysiology and interdisciplinary management. World Neurosurg 135:222–227
Al Fauzi A, Djatisoesanto W, Wahyuhadi J, Parenrengi MA, Turchan A (2017) A rare case of repeated migration and transurethral extrusion of ventriculoperitoneal shunt. J Pediatr Neurosci 12:96–98
Arsanious D, Sribnick E (2019) Intrahepatic cerebrospinal fluid pseudocyst: a case report and systematic review. World Neurosurg 125:111–116
Bansal H, Gupta G, Gupta M, Kaushal R (2015) Unusual ventriculoperitoneal (VP) shunt tube extrusion through anus in a child with Dandy-Walker malformation: a rare case report. J Clin Diagn Res 9: PD25–26
Berhouma M, Messerer M, Houissa S, Khaldi M (2008) Transoral protrusion of a peritoneal catheter: a rare complication of ventriculoperitoneal shunt. Pediatr Neurosurg 44:169–171
Cohen-Addad DI, Hewitt K, Bell D (2018) A ventriculoperitoneal shunt incidentally found in the stomach. Radiol Case Rep 13:1159–1162
Knuth J, Detzner M, Heiss MM, Weber F, Bulian DR (2013) Laparoscopy for a ventriculoperitoneal shunt tube dislocated into the colon. JSLS 17:675–678
Low SW, Sein L, Yeo TT, Chou N (2010) Migration of the abdominal catheter of a ventriculoperitoneal shunt into the mouth: a rare presentation. Malays J Med Sci 17:64–67
Saha H, Burman SS, Saha K, Ghosh D (2018) Spontaneous asymptomatic migration of ventriculoperitoneal shunt into thoracic cavity: a case report with review of literature. J Pediatr Neurosci 13:352–354
Sidhu JS, Mandal A, Kafle P, Chaulagai B, Gayam V (2019) Ventriculoperitoneal shunt migration inside the gastric lumen: a rare case report. Cureus 11: e4453
Singh S, Pant N, Kumar P, Pandey A, Khan TR, Gupta A, Rawat J (2016) Migration of ventriculoperitoneal shunt into a hernia sac: an unusual complication of ventriculoperitoneal shunt surgery in children. Pediatr Neurosurg 51:154–157
Snow RB, Lavyne MH, Fraser RA (1986) Colonic perforation by ventriculoperitoneal shunts. Surg Neurol 25:173–177
Suryadevara R, Lieber BA, Garcia E, Sood S, Haridas A, Ham S (2018) Migration of a ventriculo-peritoneal shunt catheter into a back incision of a patient with previous spinal fusion. Childs Nerv Syst 34:787–789
Sathyanarayana S, Wylen EL, Baskaya MK, Nanda A (2000) Spontaneous bowel perforation after ventriculoperitoneal shunt surgery: case report and a review of 45 cases. Surg Neurol 54:388–396
Kunitaka M, Akai T, Akioka N, Tomita T, Nagai S, Kuroda S (2018) Lacunar stroke, cavernous angioma, and fusiform aneurysm due to irradiation for pilocytic astrocytoma—a case report. J Stroke Cerebrovasc Dis 27:e165–e167
Digray NC, Thappa DR, Arora M, Mengi Y, Goswamy HL (2000) Silent bowel perforation and transanal prolapse of a ventriculoperitoneal shunt. Pediatr Surg Int 16:94–95
Guthe SP, Pravin S, Darade P, Velho V (2018) Silent migration of ventriculoperitoneal shunt per anus in a child: management and review of literature. Asian J Neurosurg 13:446–448
Ghritlaharey RK, Budhwani KS, Shrivastava DK, Gupta G, Kushwaha AS, Chanchlani R, Nanda M (2007) Trans-anal protrusion of ventriculo-peritoneal shunt catheter with silent bowel perforation: report of ten cases in children. Pediatr Surg Int 23:575–580
Brownlee JD, Brodkey JS, Schaefer IK (1998) Colonic perforation by ventriculoperitoneal shunt tubing: a case of suspected silicone allergy. Surg Neurol 49:21–24
Vuyyuru S, Ravuri SR, Tandra VR, Panigrahi MK (2009) Anal extrusion of a ventriculo peritoneal shunt tube: endoscopic removal. J Pediatr Neurosci 4:124–126
Allouh MZ, Al Barbarawi MM, Asfour HA, Said RS (2017) Migration of the distal catheter of the ventriculoperitoneal shunt in hydrocephalus: a comprehensive analytical review from an anatomical perspective. Clin Anat 30:821–830
Yang TK, Sim KB (2013) Multiple liver abscesses associated with ventriculoperitoneal shunt infection: case report and review of the literature. J Korean Neurosurg Soc 54:441–443
Yousfi MM, Jackson NS, Abbas M, Zimmerman RS, Fleischer DE (2003) Bowel perforation complicating ventriculoperitoneal shunt: creport and review. Gastrointest Endosc 58:144–148
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest concerning the materials or methods used in this study or the findings specified in this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shiro, T., Akai, T., Yamamoto, S. et al. A case of intestinal perforation with a residual shunt tube placed during childhood: should we remove the non-functioning tube?. Childs Nerv Syst 38, 1389–1392 (2022). https://doi.org/10.1007/s00381-021-05414-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-021-05414-2