Abstract
Purpose
To determine the relative efficacy of intravenous therapy for postconcussive headaches in a pediatric population, as compared to oral therapy.
Methods
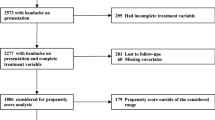
Pediatric patients treated for postconcussive headaches at an outpatient infusion clinic from 2016 to 2018 were selected for inclusion in the study. Of the 95 patients who were treated in clinic, 53 patients were selected for a retrospective chart review. Clinic visits before and after infusions were reviewed to determine changes in headache score (HA), symptom severity score (SSS), and self-reported symptom relief. An age-matched and SSS-matched group served as a control. The control group received only oral therapy for their headaches. The infusion consisted of parenteral ketorolac, compazine, diphenhydramine, and a normal saline bolus (20 mg/kg).
Results
Following infusion therapy, overall mean HA and SSS scores were both reduced (p < 0.0001). Oral therapy demonstrated a similar mean overall reduction in HA and SS scores (p < 0.0001). While both groups achieved a reduction in HA and SS scores, there was not a statistically significant difference in reduction of symptoms scores between the oral and infusion groups.
Conclusion
Infusion therapy is as effective at reducing HA and SSS as established oral therapies. Infusion therapy may have a shorter time to headache abortion than oral therapy based on pharmacokinetics. Further, some physicians are unwilling to allow an athlete to return to play while taking suppressive medication. Future studies may show that an infusion could allow a more rapid return to play and resolution of symptoms.


Similar content being viewed by others
References
Moreno MA (2012) Youth sports and concussion risk. Arch Pediatr Adolesc Med 166(4):396. https://doi.org/10.1001/archpediatrics.2012.79
Bazarian JJ, McClung J, Shah MN, Cheng YT, Flesher W, Kraus J (2005) Mild traumatic brain injury in the United States, 1998–2000. Brain Inj 19(2):85–91. https://doi.org/10.1080/02699050410001720158
Thurman DJ, Branche CM, Sniezek JE (1998) The epidemiology of sports-related traumatic brain injuries in the United States: Recent developments. J Head Trauma Rehabil 13(2):1–8. https://doi.org/10.1097/00001199-199804000-00003
Langlois JA, Rutland-Brown W, Thomas KE (2005) The incidence of traumatic brain injury among children in the United States: Differences by race. J Head Trauma Rehabil 20(3):229–238. https://doi.org/10.1097/00001199-200505000-00006
Blinman TA, Houseknecht E, Snyder C, Wiebe DJ, Nance ML (2009) Postconcussive symptoms in hospitalized pediatric patients after mild traumatic brain injury. J Pediatr Surg 44(6):1223–1228. https://doi.org/10.1016/j.jpedsurg.2009.02.027
Lucas S (2015) Posttraumatic headache: Clinical characterization and management. Curr Pain Headache Rep 19(10):48. https://doi.org/10.1007/s11916-015-0520-1
Olesen J (2018) Headache classification committee of the International Headache Society (IHS): The International Classification of Headache Disorders, 3rd edition. Cephalalgia 38(1):1–211. https://doi.org/10.1177/0333102417738202
Kacperski J, Arthur T (2016) Management of post-traumatic headaches in children and adolescents. Headache 56(1):36–48. https://doi.org/10.1111/head.12737
Lucas S (2015) Characterization and management of headache after mild traumatic brain injury. In: FH Kobeissy
Trottier ED, Bailey B, Lucas N, Lortie A (2012) Prochlorperazine in children with migraine: A look at its effectiveness and rate of akathisia. Am J Emerg Med 30(3):456–463. https://doi.org/10.1016/j.ajem.2010.12.020
Kabbouche MA, Vockell AL, LeCates SL, Powers SW, Hershey AD (2001) Tolerability and effectiveness of prochlorperazine for intractable migraine in children. Pediatrics 107(4):E62. https://doi.org/10.1542/peds.107.4.e62
Leung S, Bulloch B, Young C, Yonker M, Hostetler M (2013) Effectiveness of standardized combination therapy for migraine treatment in the pediatric emergency department. Headache 53(3):197–491. https://doi.org/10.1111/head.12042
Friedman BW, Esses D, Solorzano C et al (2008) A randomized controlled trial of prochlorperazine versus metoclopramide for treatment of acute migraine. Ann Emerg Med 52(4):399–406. https://doi.org/10.1016/j.annemergmed.2007.09.027
Kuczynski A, Crawford S, Bodell L, Dewey D, Barlow KM (2013) Characteristics of post-traumatic headaches in children following mild traumatic brain injury and their response to treatment: A prospective cohort. Dev Med Child Neurol 55(7):636–641. https://doi.org/10.1111/dmcn.12152
Orr SL, Friedman BW, Christie S et al (2016) Management of adults with acute migraine in the emergency department: The American headache society evidence assessment of parenteral pharmacotherapies. Headache 56(6):911–940. https://doi.org/10.1111/head.12835
Pinchefsky E, Dubrovsky AS, Friedman D, Shevell M (2015) Part II–management of pediatric post-traumatic headaches. Pediatr Neurol 52(3):270–280. https://doi.org/10.1016/j.pediatrneurol.2014.10.015
Kinnaman KA, Mannix RC, Comstock RD, Meehan 3rd WP (2013) Management strategies and medication use for treating paediatric patients with concussions. Acta paediatrica (Oslo, Norway: 1992) 102(9):424–428. https://doi.org/10.1111/apa.12315
Jones J, Sklar D, Dougherty J, White W (1989) Randomized double-blind trial of intravenous prochlorperazine for the treatment of acute headache. JAMA 261(8):1174–1176
Thomas SH, Stone CK, Ray VG, Whitley TW (1994) Intravenous versus rectal prochlorperazine in the treatment of benign vascular or tension headache: A randomized, prospective, double-blind trial. Ann Emerg Med 24(5):923–927. https://doi.org/10.1016/s0196-0644(54)00222-3
Chan S, Kurowski B, Byczkowski T, Timm N (2015) Intravenous migraine therapy in children with posttraumatic headache in the ED. Am J Emerg Med 33(5):635–639. https://doi.org/10.1016/j.ajem.2015.01.053
Kabocha M (2015) Management of pediatric migraine headache in the emergency room and infusion center. Headache 55(10):1365–1370. https://doi.org/10.1111/head.12694
Friedman BW, Babbush K, Irizarry E, White D, John GE (2018) An exploratory study of IV metoclopramide + diphenhydramine for acute post-traumatic headache. Am J Emerg Med 36(2):285–289. https://doi.org/10.1016/j.ajem.2017.10.034
Montgomery SA (1997) Suicide and antidepressants. Ann N Y Acad Sci 836:329–338. https://doi.org/10.1111/j.1749-6632.1997.tb52368.x
Thanacoody HKR, Thomas SHL (2005) Tricyclic antidepressant poisoning: Cardiovascular toxicity. Toxicol Rev 24(3):205–214. https://doi.org/10.2165/00139709-200524030-00013
Heyer GL, Idris SA (2014) Does analgesic overuse contribute to chronic post-traumatic headaches in adolescent concussion patients? Pediatr Neurol 50(5):464–468. https://doi.org/10.1016/j.pediatrneurol.2014.01.040
Mihalik JP, Stump JE, Collins MW, Lovell MR, Field M, Maroon JC (2005) Posttraumatic migraine characteristics in athletes following sports-related concussion. J Neurosurg 102(5):850–855. https://doi.org/10.3171/jns.2005.102.5.0850
Kontos AP, Elbin RJ, Lau B et al (2013) Posttraumatic migraine as a predictor of recovery and cognitive impairment after sport-related concussion. Am J Sports Med 41(7):1497–1504. https://doi.org/10.1177/0363546513488751
Desai N, Wiebe DJ, Corwin DJ, Lockyer JE, Grady MF, Master CL (2019) Factors affecting recovery trajectories in pediatric female concussion. Clin J Sport Med: Official Journal of the Canadian Academy of Sport Medicine 29(5):361–367. https://doi.org/10.1097/JSM.0000000000000646
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pate, J., Mooney, J., Katz, E. et al. Efficacy of outpatient infusion therapy in pediatric patients with postconcussive headaches. Childs Nerv Syst 38, 103–108 (2022). https://doi.org/10.1007/s00381-021-05383-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-021-05383-6