Abstract
Study design
Case series, literature review, and technical note.
Objectives
To compare two different approaches to treat the spinal deformity with split cord malformation type I (SCM I). To present a new method of one-stage surgical treatment of congenital spinal deformity with wide bony septum (SCM I).
Methods
Analysis of the literature on the different types of combined surgical treatment of spinal deformities with SCM I was performed. We have provided our own data on 27 patients treated for congenital spinal deformity and SCM I, one of which underwent Schwab IV type osteotomy at the apex of the deformity through the bony septum and pedicles. Inclusion criteria were presence of spinal deformity in combination with SCM 1, performed surgery to correct spinal deformity, and follow-up period of at least 2 years.
Results
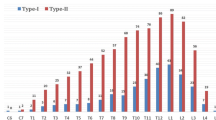
The result of the literature review was controversial and requires additional research. The average age of patients was 8.8 ± 6.6 years old. One-stage treatment of SCM I and spinal deformity was performed in 10 patients (group I) and two-stage in 14 patients (group II). Three patients with severe myelodysplasia, SCM I, and congenital kyphoscoliosis underwent correction of spinal deformity without SCM I removing (group III). The group I had the longest surgery duration (mean 289 ± 75 min) and largest blood loss (mean 560 ± 386 ml), a high percentage of deformity correction (mean 69.6%), and the highest rate of complications (60%). The most optimal was the two-stage treatment with the mean surgery duration 191 ± 137 min, mean blood loss 339 ± 436 ml, mean correction rate 63%, and frequency of complications 21%. The average follow-up time was 6.0 ± 2.6 years.
Conclusions
One stage surgery associated with a large surgical invasion and a large number of complications. It can be used in some cases, for example when the wide bony septum (SCM I) is localized at the apex of the congenital scoliosis or kyphosis. In all other cases, it is worth adhering to a two-stage treatment. Many new works demonstrate the relative safety and effectiveness of deformity correction without removing the SCM. In our opinion, indications for treatment of spinal deformity without SCM I removing can be the need to perform a shortening ostetomy outside the SCM zone. The remaining cases require a thorough assessment and a balanced decision.




Similar content being viewed by others
References
Hui H, Tao HR, Jiang XF, Fan HB, Yan M, Luo ZJ (2012) Safety and efficacy of 1-stage surgical treatment of congenital spinal deformity associated with split spinal cord malformation. Spine 37(25):2104–13. Epub 01/06/2012. https://doi.org/10.1097/BRS.0b013e3182608988. PubMed PMID: 22648030
Pierre-Aurelien B, Federico DR, Alexandru S, Carmine M (2018) Management of split cord malformation in children: The Lyon experience. Child’s Nervous System 34(5):883–891. https://doi.org/10.1007/s00381-018-3772-3
Rajasekaran S, Kamath V, Kiran R, Shetty AP (2010) Intraspinal anomalies in scoliosis: An MRI analysis of 177 consecutive scoliosis patients. Indian J Orthop 44(1):57–63. Epub 19/02/2010. https://doi.org/10.4103/0019-5413.58607. PubMed PMID: 20165678; PubMed Central PMCID: PMCPMC2822421
Shen J, Wang Z, Liu J, Xue X, Qiu G (2013) Abnormalities associated with congenital scoliosis: A retrospective study of 226 Chinese surgical cases. Spine (Phila Pa 1976) 38(10):814–8. Epub 01/12/2012. https://doi.org/10.1097/BRS.0b013e31827ed125. PubMed PMID: 23197014
Pang D, Dias MS, Ahab-Barmada M (1992) Split cord malformation: Part I: A unified theory of embryogenesis for double spinal cord malformations. Neurosurgery 31(3):451–80. Epub 01/09/1992. https://doi.org/10.1227/00006123-199209000-00010. PubMed PMID: 1407428
Tortori-Donati P, Rossi A, Cama A (2000) Spinal dysraphism: A review of neuroradiological features with embryological correlations and proposal for a new classification. Neuroradiology 42(7):471–91. Epub 22/08/2000. https://doi.org/10.1007/s002340000325. PubMed PMID: 10952179
Kobets AJ, Oliver J, Cohen A, Jallo GI, Groves ML (2021) Split cord malformation and tethered cord syndrome: case series with long-term follow-up and literature review. Child’s nervous system: ChNS: Official Journal of the International Society for Pediatric Neurosurgery 37(4):1301–6. Epub 27/11/2020. https://doi.org/10.1007/s00381-020-04978-9. PubMed PMID: 33242106
Chen B, Yuan Z, Chang MS, Huang JH, Li H, Yang WZ et al (2015) Safety and efficacy of one-stage spinal osteotomy for severe and rigid congenital scoliosis associated with split spinal cord malformation. Spine 40(18):E1005–13. Epub 15/07/2015. https://doi.org/10.1097/brs.0000000000001039. PubMed PMID: 26165211
Winter RB, Haven JJ, Moe JH, Lagaard SM (1974) Diastematomyelia and congenital spine deformities. J Bone Joint Surg Am 56(1):27–39 (Epub 01/01/1974 PubMed PMID: 4812165)
Beuriat PA, Di Rocco F, Szathmari A, Mottolese C (2018) Management of split cord malformation in children: The Lyon experience. Childs Nerv Syst 34(7):1433. Epub 19/05/2018. https://doi.org/10.1007/s00381-018-3813-y. PubMed PMID: 29774384
Feng F, Shen J, Zhang J, Zhao H, Zhao Y, Li Z et al (2016) Clinical outcomes of different surgical strategy for patients with congenital scoliosis and type I split cord malformation. Spine 41(16):1310–6. Epub 26/02/2016. https://doi.org/10.1097/brs.0000000000001530. PubMed PMID: 26913465
Hui H, Zhang ZX, Yang TM, He BR, Hao DJ (2014) Vertebral column resection for complex congenital kyphoscoliosis and type I split spinal cord malformation. European spine journal : Official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society 23(6):1158–63. Epub 16/11/2013. https://doi.org/10.1007/s00586-013-3044-6. PubMed PMID: 24232596
Zhao Q, Shi B, Sun X, Liu Z, Su H, Li Y et al (2019) Do untreated intraspinal anomalies in congenital scoliosis impact the safety and efficacy of spinal correction surgery? A retrospective case-control study. J Neurosurg Spine 31(1):40–5. Epub 06/04/2019. https://doi.org/10.3171/2019.1.Spine181205. PubMed PMID: 30952134
Zhang HQ, Deng A, Liu SH, Wang YX, Alonge E (2020) Posterior-only surgical correction with heavy halo-femoral traction for the treatment of severe and rigid congenital scoliosis associated with tethered spinal cord and type II split cord malformation. World Neurosurg 139:e151-e8. Epub 07/04/2020. https://doi.org/10.1016/j.wneu.2020.03.145. PubMed PMID: 32251829
Jayaswal A, Kandwal P, Goswami A, Vijayaraghavan G, Jariyal A, Upendra BN et al (2016) Early onset scoliosis with intraspinal anomalies: management with growing rod. European spine journal: Official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society 25(10):3301–7. Epub 14/04/2016. https://doi.org/10.1007/s00586-016-4566-5. PubMed PMID: 27072552
Liu X, Yuan S, Tian Y, Wang L, Zheng Y, Li J (2015) Expanded eggshell procedure combined with closing-opening technique (a modified vertebral column resection) for the treatment of thoracic and thoracolumbar angular kyphosis. J Neurosurg Spine 23(1):42–8. Epub 25/04/2015. https://doi.org/10.3171/2014.11.Spine14710. PubMed PMID: 25909274
Ayvaz M, Akalan N, Yazici M, Alanay A, Acaroglu RE (2009) Is it necessary to operate all split cord malformations before corrective surgery for patients with congenital spinal deformities? Spine 34(22):2413–8. Epub 16/10/2009. https://doi.org/10.1097/BRS.0b013e3181b9c61b. PubMed PMID: 19829255
Zhang H-Q, Deng A, Tang M-X, Liu S-H, Wang Y-X, Gao Q-L (2020) Posterior-only surgical correction with heavy halo-femoral traction for the treatment of rigid congenital scoliosis associated with split cord malformation. BMC Musculoskeletal Disorders 21(1). https://doi.org/10.1186/s12891-020-3124-9
Huang Z, Li X, Deng Y, Sui W, Fan H, Yang J et al (2019) The treatment of severe congenital scoliosis associated with type I split cord malformation: Is a preliminary bony septum resection always necessary? Neurosurgery 85(2):211–22. Epub 31/07/2018. https://doi.org/10.1093/neuros/nyy237. PubMed PMID: 30060239
Yang N, Luo M, Yu Y, Wang J, Xia L, Wang W (2019) Is it better to resect a bony spur before corrective surgery for congenital scoliosis with type I split cord malformation? World Neurosurg 125:e1151-e9. Epub 23/02/2019. https://doi.org/10.1016/j.wneu.2019.01.265. PubMed PMID: 30790730
Shen J, Zhang J, Feng F, Wang Y, Qiu G, Li Z (2016) Corrective surgery for congenital scoliosis associated with split cord malformation: It may be safe to leave diastematomyelia untreated in patients with intact or stable neurological status. J Bone Joint Surg Am 98(11):926-36. Epub 03/06/2016. PubMed PMID: 27252437
Feng F, Shen J, Zhang J, Li S, Yu K, Tan H (2016) Characteristics and clinical relevance of the osseous spur in patients with congenital scoliosis and split spinal cord malformation. J Bone Joint Surg Am 98(24):2096–102. Epub 22/12/2016. https://doi.org/10.2106/jbjs.16.00414. PubMed PMID: 28002373
Lewandrowski KU, Rachlin JR, Glazer PA (2004) Diastematomyelia presenting as progressive weakness in an adult after spinal fusion for adolescent idiopathic scoliosis. The spine journal: Official Journal of the North American Spine Society 4(1):116–9. Epub 30/01/2004. https://doi.org/10.1016/j.spinee.2003.08.028. PubMed PMID: 14749200
Saifutdinov M, Skripnikov A, Savin D, Ochirova P, Tret’iakova A (2017) Methodological problems of intraoperative neuromonitoring during operative correction of spinal deformity (literature review). Genij Ortopedii 23(1):102–110
Schwab F, Blondel B, Chay E, Demakakos J, Lenke L, Tropiano P et al (2015) The comprehensive anatomical spinal osteotomy classification. Neurosurgery 76 Suppl 1:S33–41; discussion S. Epub 19/02/2015. https://doi.org/10.1227/01.neu.0000462076.73701.09. PubMed PMID: 25692366
Obeid I, Bourghli A, Boissière L, Vital JM, Barrey C (2014) Complex osteotomies vertebral column resection and decancellation. European Journal of orthopaedic surgery & traumatology: Orthopedie traumatologie 24(1):S49–57. Epub 17/05/2014. https://doi.org/10.1007/s00590-014-1472-6. PubMed PMID: 24831304
Boriani S, Bandiera S, Colangeli S, Ghermandi R, Gasbarrini A (2014) En bloc resection of primary tumors of the thoracic spine: Indications, planning, morbidity. Neurol Res 36(6):566–76. Epub 15/04/2014. https://doi.org/10.1179/1743132814y.0000000369. PubMed PMID: 24725289
Dang L, Liu Z, Liu X, Jiang L, Yu M, Wu F et al (2020) Sagittal en bloc resection of primary tumors in the thoracic and lumbar spine: Feasibility, safety and outcome. Scientific reports 10(1):9108. Epub 06/06/2020. https://doi.org/10.1038/s41598-020-65326-0. PubMed PMID: 32499491; PubMed Central PMCID: PMCPMC7272461 Hospital (BYSY 2017001)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript. The authors declare no conflict of interest in this work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sergeenko (Pavlova), O.M., Savin, D.M. & Ryabykh, S.O. Treatment of spinal deformity with diastematomyelia type I: one-stage, two-stage surgery and new technique (vertebral column resection through wide bony septum). Childs Nerv Syst 38, 163–172 (2022). https://doi.org/10.1007/s00381-021-05382-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-021-05382-7